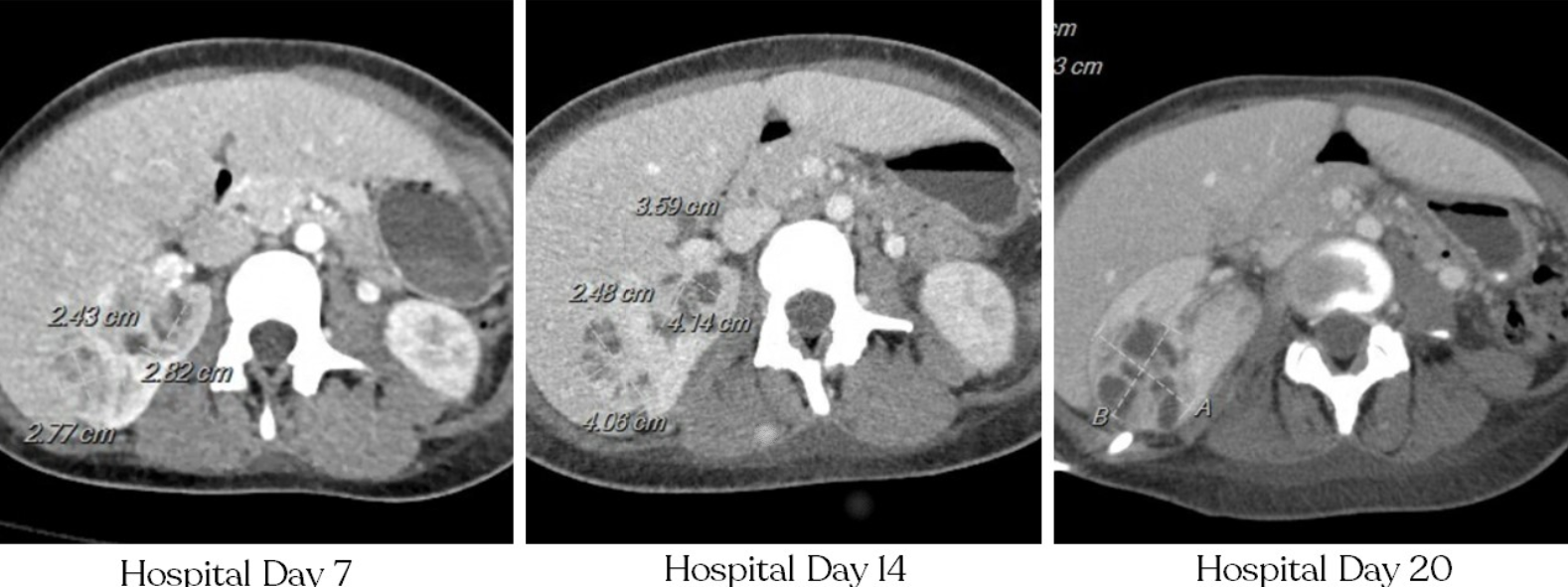
Case Presentation: A 23-year-old- female with a past medical history of neuromyelitis optica on rituximab and hydronephrosis was found to have a culture-negative renal abscess. She had first presented 4 months prior at 26 weeks of pregnancy with complaints of a painful mass in her urethra, and right hydronephrosis was seen on CT. Prior to this, she had been treated for gonorrhea, and repeat testing was negative. A urethral diverticulectomy was performed and a foley catheter was placed. She was also found to have nephrotic range proteinuria and hematuria at that time. Testing for IgA nephropathy and other autoimmune etiologies were negative. Her pregnancy was complicated by preterm premature rupture of the membranes with premature labor at 29 weeks requiring C-section. Post-partum she continued to have chronic pelvic discomfort, bladder spasms, and dysuria. Ten days prior to admission, cystourethroscopy showed a friable, erythematous vaginal vault with a large opening of the anterior vaginal wall. She presented to the hospital with low back pain, nausea, and fevers. She was febrile and tachycardic. CT showed bilateral hydroureteronephrosis, urothelial enhancement, and possible pyelonephritis. Urinalysis showed moderate leukocyte esterase, protein 500mg/dl, large blood, >100 RBC/HPF, >100 WBC/HPF, and many WBC clumps. Urine culture grew mixed flora. Blood cultures on admission grew S. epidermis in both cultures. Nephrostomy tubes were placed. A transthoracic echocardiogram did not show valvular lesions or regurgitation. She continued to fever to 39C with leukocytosis despite treatment with broad spectrum antibiotics. Multiple repeat blood and urine cultures were without growth. Urinalysis showed continued pyuria. Repeat CT scan showed a renal abscess which expanded on repeat imaging. Multiple abscess aspirations were without growth in aerobic/anaerobic, fungal, and AFB cultures. PCR testing from the abscess aspiration was positive for Ureaplasma urealyticum.
Discussion: Ureaplasma urealyticum is a small bacterium which cannot be seen on gram stain due to the lack of a cell wall. It does not grow on routine culture medium. It is present in the vaginal flora of 40-80% of sexually active women and causes up to 30% of non-gonococcal urethritis. Ureaplasma is also associated with surgical site infections, PPROM, and invasive infections in transplant recipients. In one study, hypogammaglobulinemia or rituximab was associated with 71% of invasive Ureaplasma infections in non-transplant patients. There are rare reports of Ureaplasma urealyticum causing renal abscesses. Due to lack of a cell wall, Ureaplasma will not respond to most antibiotics and should be treated with tetracyclines, macrolides, or fluroquinolones.
Conclusions: Conclusion: In patients with sterile pyuria and urethritis, Ureaplasma urealyticum infection should be considered. Organ transplant and hypogammaglobinemia are associated with invasive infection which can rarely manifest as a renal abscess. In this case, the lack of response to broad spectrum antibiotics and negative cultures in a patient on rituximab caused the clinician to consider invasive Ureasplasma infection.