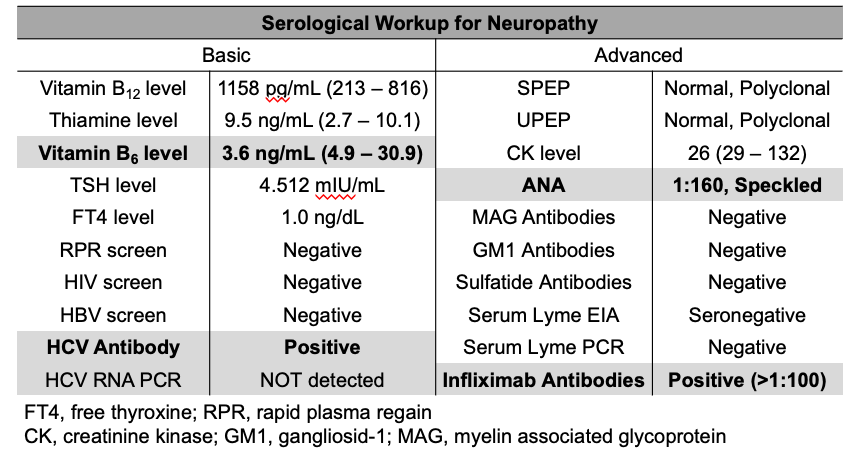
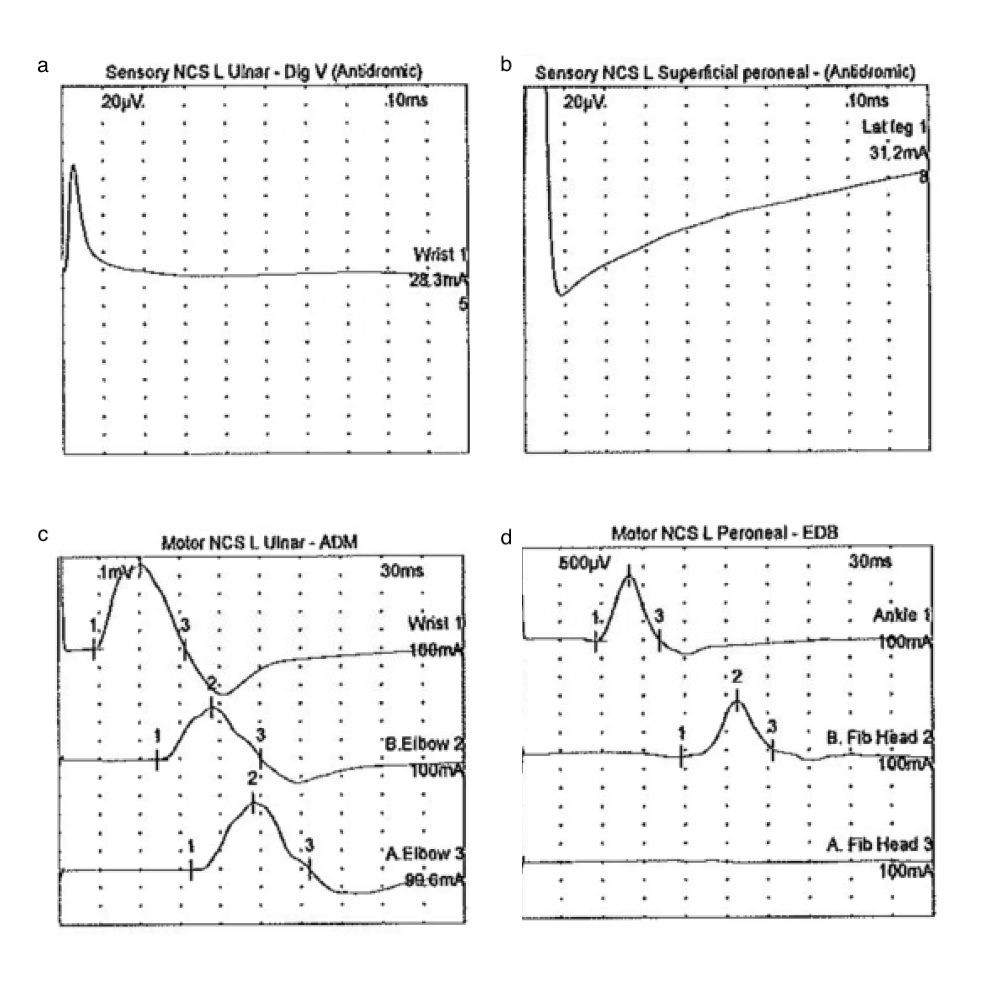
Case Presentation: A 66-year-old female with a history of Crohn’s disease (CD) and Stage IV chronic kidney disease presented with a 2-day history of acute-onset numbness and tingling of bilateral hands and feet. The patient has a long-standing history of CD and underwent a right hemicolectomy with end ileostomy at the age of 13. She had a CD flare 5 months ago manifested as interstitial lung disease and diversion colitis, for which she was treated with high-dose steroids followed by infliximab as a steroid-sparing agent. She completed 5 mg/kg doses at Week 0, 2 and 6, and remained on every-8-week dosing with most recent one completed 5 weeks before admission. Physical examination showed significant symmetrical muscle weakness, with muscle strength 3/5 on proximal upper extremities (UEs), 4/5 distal UEs, 2/5 proximal lower extremities (LEs), and 4/5 distal LEs; areflexia was also noticed in bilateral LEs. Cranial nerve functions were intact. Routine laboratory tests showed a normal white cell count, baseline elevated creatinine, and mild inflammation with a CRP (2.80 mg/dL). Testing for thyroid function, vitamin B12, vitamin B1, folate, creatinine kinase (CK), syphilis, HIV and tuberculosis all returned normal (Table 1). Guillain-Barré syndrome (GBS) was highly suspected, electromyography (EMG) was obtained and demonstrated acute sensorimotor axonal neuropathy evidenced by the absence of left median, ulnar, sural and peroneal sensory potentials as well as low amplitude and borderline velocities of left ulnar, peroneal and tibial motor potentials with decreased recruitment. GBS was diagnosed based on history, examination, and characteristic EMG findings. Further tests for antibodies against ganglioside (GM1), myelin-associated glycoprotein (MAG), and sulfatide were negative. Patient was treated with intravenous immunoglobulin (IVIG) for 5 days; she had significant neurologic improvement and was discharged with follow-up for further discussion on anti-TNF therapy cessation.
Discussion: Tumor necrosis factor antagonists including infliximab and adalimumab are widely used in the treatment of inflammatory bowel disease (IBD). Anti-tumor necrosis factor (anti-TNF) medications have been reported to carry the risk of unmasking or aggravating demyelinating disorders such as multiple sclerosis. However, Guillain-Barré syndrome (GBS) is a less recognized but potentially debilitating immune-mediated neurological disorder that has also been described in association with anti-TNF therapy. We present a rare case of GBS associated with Infliximab therapy in a patient with severe Crohn’s disease (CD). Although the pathophysiology behind the association between GBS and anti-TNF agents is not well understood, one hypothesis for the mechanism involves anti-TNF therapy unmasking latent infections or increasing susceptibility to infections that may trigger GBS through molecular mimicry.
Conclusions: GBS is a rare but potentially serious complication associated with anti-TNF therapy. As such, clinical suspicion for GBS needs to be high in patients with sensory changes, motor weakness, areflexia or ataxia in the setting of anti-TNF therapy. Prompt neurological consultation, initiation of IVIG, and cessation of anti-TNF therapy will help prevent debilitating neurological deficits.