Background: Choroidal melanoma, the most common primary intraocular malignancy in adults, is a dangerous cancer which can lead to blindness. Diagnosed at an average age of 65 & lacking identifiable environmental or genetic factors, melanoma of the eye can affect anyone. Commonly found on routine ophthalmological screening, patients are sent to quaternary hospitals for further evaluation by an ocular oncology specialist. Ocular oncologists evaluate these patients and based on size and characteristics of the tumor helps patients decide on treatment options: brachytherapy with radioactive eye plaque or enucleation. If brachytherapy is chosen, a radiation oncologist needs to create a radioactive eye plaque for surgical use. The patient presents for surgery on the pre-specified day, undergoes surgery and is admitted to the hospital.
Purpose: At our academic institution, our hospitalist department worked in conjunction with our ocular & radiation oncologists to create a value stream process map & checklist to reduce redundancy and create a co-managed model of care for this very specialized subset of patients.
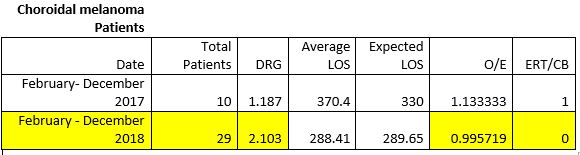
Description: Beginning in February of 2018, we deployed a co-managed model of care for this specialized subset of patients. In our co-managed model, patients identified with choroidal melanoma would be evaluated in the outpatient setting by our ocular oncologist and a surgical plan would be created with the assistance of our predetermined radiation oncologist. On the day of surgery, the patient would be admitted to the pre-operative area under the ocular ophthalmologist and undergo surgery. Post-surgery, the patient would be admitted to the cancer hospitalist service. Post-surgical care was focused on pain control, adherence to eye drops, and co-morbidity management. On post-operative day #4, the patient would return to the operating room and have the radioactive plaque removed and be discharged from the cancer hospitalist service. The AIM of the co-managed service was to reduce adverse patient events by 50% & reduce length of stay (LOS) to < 1 over the course of 2018.
Conclusions: As noted in the table, the co-managed service was able to improve LOS to < 1. In addition, patients admitted to the co-managed service had zero emergency response teams (ERT) or code blues called. An added benefit of the co-managed service was the increase in DRG billing due to hospitalist documentation & increased surgical volume due to our ocular ophthalmologist having time freed up to focus on clinic and the operating room.