Background: The Joint Commission (TJC) defines a sentinel event as one related to patient safety resulting in death, permanent, or severe harm.(1) In TJC Sentinel Event Data Annual Review for 2022, communication breakdowns were identified as the root cause for these events. With stricter duty hour restrictions in hospitals nationally, the number of patient caregivers and thus handoffs between providers have increased, leading to an increased chance for sentinel events to occur. Standardizing the patient handoff process can improve patient outcomes and reduce medical errors. (2, 3, 4)
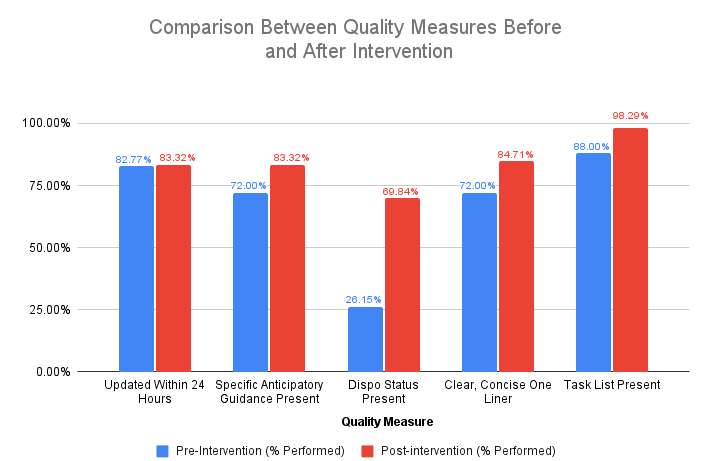
Purpose: To improve the quality of written handoffs in our Internal Medicine residency program by increasing the inclusion of daily updates from 80% to 90%, patient-specific anticipatory guidance from 70% to 90%, and disposition status from 25% to 35% within two months of implementing a standardized handoff curriculum.
Description: Based on resident feedback, a committee was assembled to review handoffs. Preliminary chart review was performed assessing our primary metrics: 1) Updated within 24 hours, 2) Included patient-specific anticipatory guidance, and 3) Included disposition status (i.e. high risk of decompensation denoted as “Watcher,” ICU Downgrade, Medically Active, or Pending Discharge). Secondary metrics included a subjective review of the quality of the one-liner, and the inclusion of a task list for the team. An electronic medical record (EMR) smart phrase was created to standardize handoffs. A two-part intervention included interactive workshops during resident didactics and the introduction of the EMR smart phrase (Figure 1). Prior to the intervention, a total of 325 charts were reviewed. The primary outcomes of handoffs updated within 24 hours, having patient specific anticipatory guidance, and having patient disposition status were performed 82.8%, 72.0%, and 26.1% of the time, respectively (Figure 2). Secondary outcomes reviewing the quality of the one-liner and presence of task lists were performed 72.0% and 88.0% of the time, respectively. Post-intervention chart review was performed weekly for eight weeks to evaluate improvement in handoff quality, with a total of 935 charts reviewed. The primary outcomes of handoffs updated within 24 hours, patient specific anticipatory guidance, and patient disposition status were performed 83.3% (increase of 0.5%), 83.3% (increase of 11.3%), and 69.8% (increase of 43.7%) of the time, respectively (Figure 2). Secondary outcomes for quality of one-liner and presence of task lists were increased by 12.7% and 10.3%, respectively. Overall, there was an increase for all metrics analyzed post-intervention, the largest being in the presence of specific anticipatory guidance and patient disposition status. Project limitations included resident participation in utilizing the EMR smart phrase, as well as the subjective aspect of the secondary outcomes, based on reviewer.
Conclusions: Following the implementation of a standardized handoff tool and focused education in the largest Internal Medicine Residency Program in the country, written handoffs provided a more accurate picture of patients’ clinical status. By fostering better communication among providers, comprehensive handoffs increase the confidence of the oncoming team in patient care, enabling them to make informed decisions quickly, and preventing errors. The next phase of this project will include incorporating resident feedback to further develop the smart phrase and increase use of the standardized format.