Case Presentation: A 38-year-old woman with well-controlled Crohn’s disease on immunosuppression presented to the emergency department with a three- day history of rash and fevers following antimicrobial treatment at an outside urgent care facility for presumed bacterial sinusitis. At the urgent care facility, she had received intramuscular ceftriaxone, oral azithromycin, and oral prednisone. The following day she awoke with an erythematous, maculopapular rash on her face that soon developed into pustules and spread to her trunk, back, and groin. The rash was initially pruritic but progressively became painful. She had no prior history of allergic reactions or known medication allergies. She reported burning around the eyes but no blurry vision, vision changes, or discomfort involving the eyes. She had fevers with Tmax 39.4.VS: 37.3 153/89 110 18 97% HEENT: Normal visual fields, normal visual acuity. Conjunctival injection and desquamation of bilateral upper and lower eyelid. Mucous membranes pink with diffuse desquamation of oral mucosa, lips, and tongue. Erythematous hard palate with discernable lesions.Rash: Generalized, diffuse dusky patches over her head, neck, arms, and trunk. Her upper legs had shallow, cutaneous erosions and a positive Nikolsky sign. Pinpoint, monomorphic pustules scattered on the face, torso, proximal upper extremities.GU: Diffuse tenderness to palpation throughout the vaginal wall. Erosions within the vaginal mucosa as well as on the perineum at the 6 o’clock position of the anus.Labs: Mild leukopenia (3.4). Electrolytes, creatinine, liver enzymes were normal. Urinalysis bland.Imaging: Chest X-Ray normal.The patient’s initial rash with pinpoint pustules was most consistent with acute generalized exanthematous pustulosis (AGEP), but the development of mucocutaneous involvement was highly concerning for Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis (SJS/TEN). She was transferred to the medical intensive care unit where she received IV fluid, cyclosporine via nasogastric tube, topical prednisolone, antimicrobial eye drops, and artificial tears. Dermatology and Ophthalmology were consulted and a punch biopsy was performed.She developed mild transaminitis with moderate CPK elevations, without symptoms of muscle pain, weakness, nor complications of acute renal injury. Labs and rash improved with supportive care over the following one to two weeks. She was discharged 14 days later on a cyclosporine taper and has since experienced significant improvement in her skin, eyes, and mouth.
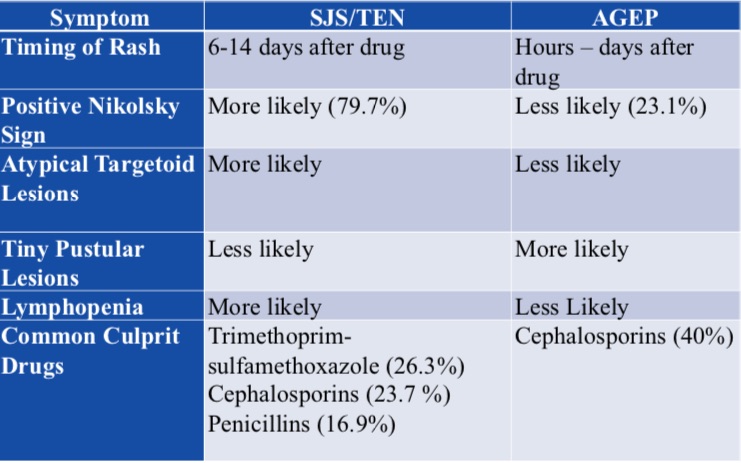
Discussion: SJS/TEN and AGEP are both classified as severe cutaneous adverse reactions (SCARs), which are life-threatening reactions usually precipitated by medications. 1, 2 SJS/TEN is difficult to distinguish from other SCARs including AGEP, but both typically have clinical findings of high-grade fever associated with the onset of a rash. 2, 3
Conclusions: An SJS/AGEP Overlap syndrome can occur; it’s important to recognize the evolution of signs and symptoms consistent with SJS/TEN even if initial presentation appears more benign.1, 2, 3Antibiotics are lifesaving but can cause significant harm through a variety of adverse events, including SCARs. The regimen of ceftriaxone/azithromycin is frequently used to treat community-acquired pneumonia, one of the most common diagnoses associated with antibiotic overuse.4Accurately weighing the risk of severe adverse effects with the potential benefit is crucial for each prescribing decision.5