Case Presentation: A 52 y.o with a past medical history of uncontrolled, untreated hypertension presented to our hospital with a 3 week history of progressively worsening lower extremity edema and shortness of breath. Review of systems was positive for hoarse voice x6 months, unintentional weight gain, cold intolerance, abdominal fullness, and cough productive of white sputum. He has a 30 pack year smoking history and endorsed regular use of marijuana and methamphetamines.
Vitals showed BP 184/124, MAP 132, and RR 20. He was afebrile, nontachycardic, with oxygen saturation of 97% on room air. Physical exam was significant for distant heart sounds, voice gargling, diffuse rhonchi, expiratory wheezing, distended abdomen, warm, dry skin, 2+ pitting edema in bilateral lower extremities, pretibial myxedema, and 25 mmhg paradoxical hemodynamic instability.
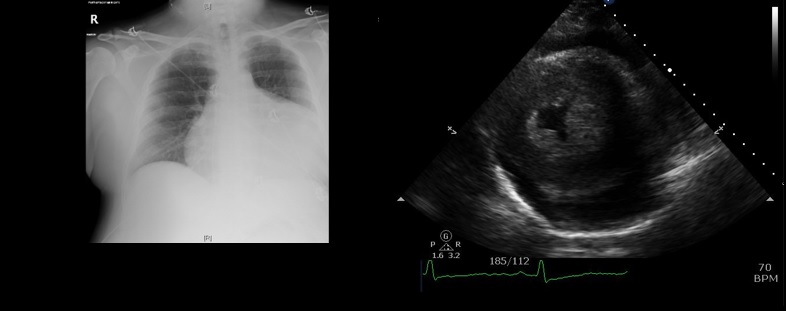
CBC was normal and CMP was significant for mild hypokalemia. CHF peptide was elevated serial troponins were slightly elevated which was later attributed to troponin leak. EKG was significant for lateral T wave inversion with low left ventricle voltage. Chest X-ray was significant for moderate pericardial effusion vs cardiomegaly and a bedside echo confirmed pericardial effusion. The patient was started on aspirin, beta blocker, high intensity statin, and prn hydralazine.
The collective findings of the chest xray, bedside echo, and physical exam put hypothyroidism high on the differential and thyroid studies were ordered with TSH 200, free T4 0.2, thyroid stimulating immunoglobulins 138, and thyroid peroxidase antibodies were >1300. He was diagnosed with severe hypothyroidism and myxedema secondary to Hashimoto thyroiditis and started on IV synthroid.
Transthoracic echocardiogram was obtained and significant for large circumferential pericardial effusion and early diastolic right heart collapse with respiratory variation of tricuspid and mitral flow velocities indicative of tamponade physiology, and severe left ventricular hypertrophy. Cardiothoracic surgery performed emergent open pericardial window initially draining 1100cc of serous fluid. He failed extubation due to acute hypoxic and hypercapneic respiratory failure secondary to rapidly progressing macroglossia which was subsequently found to be a complication of his severe hypothyroidism.
Discussion: Pericardial effusion is a well known manifestation of moderate to severe hypothyroidism with an incidence of 30-80%%, however, the progression to cardiac tamponade is a rare with roughly 20 cases reported in the literature. Historically, the treatment of hypothyroidism induced cardiac tamponade is thyroxine supplementation. In rare circumstances, pericardiocentesis and even more rarely, pericardial window is needed in a severely symptomatic patient. Our patient presented with cardiac tamponade which is an unusual presentation of hypothyroidism.
Conclusions: Evaluation of hypothyroidism is often overlooked during the initial evaluation of patients presenting with cardiac tamponade. Cardiac tamponade is life-threatening and it is important to collect a thorough history and physical and strongly consider hypothyroidism in patients, such as ours presenting with cardiac tamponade without sinus tachycardia.