Background: Adolescents have poor access to preventive care and outpatient providers face many barriers to addressing sexual health with adolescents. Recent literature advises providers to address sexual health in nontraditional settings including emergency department (ED) visits and hospitalizations. In our previous work we identified missed opportunities to address sexual health on the hospital medicine service, then implemented solutions to increase sexual history documentation, sexually transmitted infection (STI) testing, and provision of condoms or birth control. We sought to investigate adolescent patients’ experiences with these interventions.
Methods: Cross-sectional survey was conducted over a 7-month period of adolescent patients ages 13-17 after discharge from hospital medicine service at a tertiary academic children’s hospital. Survey inquired about receipt of patient-centered and confidential care; discussion of sexual health topics (contraception, STI and HIV testing, sexual orientation) with provider during hospitalization; patients’ perceptions of these discussions; and sexual history and risk behaviors.
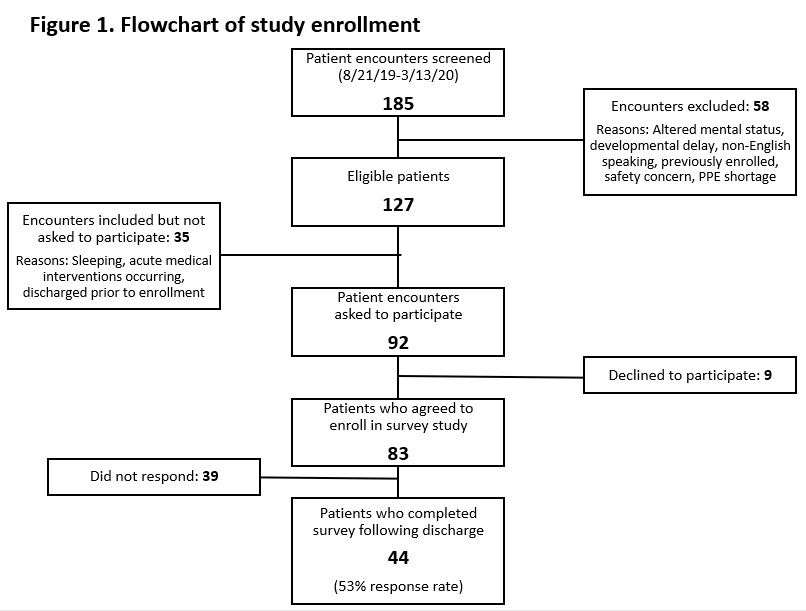
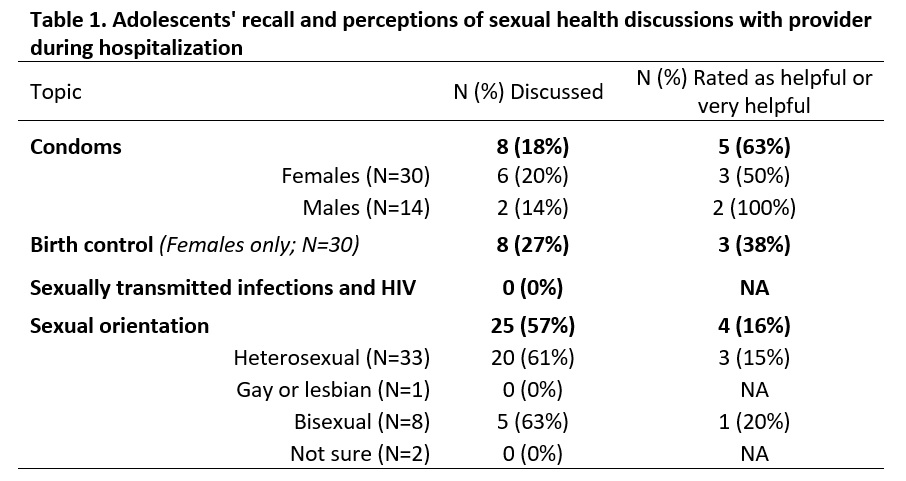
Results: 83 patients were enrolled during hospitalization and 44 completed the survey after discharge (53% total; 68% female; median age 15 (IQR 14-16 years) (Figure 1). Ten patients (23%) reported ever having had sexual intercourse with nine patients reporting they had in the past three months. No patients reported being given condoms prior to discharge; 1 female patient was prescribed birth control. Thirty-four patients (77%) reported speaking with a doctor privately about sexual health while at the hospital (32 while hospitalized; 2 in ED only). When responding to questions regarding discussions of specific health topics during hospitalization, 27% reported talking about birth control (females only); 18% about condoms; and 57% about sexual orientation. When asked to rate perceived helpfulness of these 4 discussion items, each discussion item was rated as helpful or very helpful between 16% to 63% of the time (Table 1). When responding to if STI and HIV testing discussions occurred during the hospitalization, 11 patients (25%) stated these discussions occurred only in the ED, one respondent said she could not remember, and all other respondents said the discussion never happened.
Conclusions: The percentage of patients who reported speaking with a doctor privately about sexual health (77%) corresponded well to our previous work in which we found sexual history documentation increased to 80% or more consistently. Although condoms were available for all patients as part of our improvement work, none surveyed reported receiving condoms during their hospital stay. Only a small proportion of patients recalled discussing specific topics such as contraception and STI testing. An even smaller proportion of patients reported these discussions to be helpful. By asking adolescent patients about their experiences we identified substantial opportunities for continued improvement specifically in the content and quality of sexual health care discussions. Our work highlights the importance of incorporating patient-reported data into improvement work on adolescent sexual health care provision to ensure providers in nontraditional settings are addressing this gap in a meaningful way.