Background: The transfer of patients between hospitals, i.e., interhospital transfer (IHT), introduces discontinuity of care including gaps in information transfer, which may worsen patient outcomes. In this study we aim to identify gaps in information exchange during IHT of medical patients from transferring hospitals of varying affiliation and electronic health record (EHR) integration to a tertiary referral hospital using mixed methodology.
Methods: We included all patients transferred from three acute care hospitals to the general medicine, cardiology, oncology, and ICU services at an 800-bed tertiary care facility between 11/2022-11/2023. The three transferring hospitals represent varying levels of hospital affiliation and EHR integration with the receiving hospital: Hospital 1- same health system, shared EHR; Hospital 2- different health system, accessible EHR; Hospital 3- different health system, different EHR. We used a daily generated report to identify eligible IHT patients and their corresponding admitting clinicians who were emailed REDCap surveys to complete. Survey questions inquired about the availability of patient information during transfer (i.e., the presence of erroneous or missing information) and evaluated the efficiency of patient care planning and management (i.e., spending extra time learning about the patient and next steps for care). We descriptively report the frequency of dichotomized responses to survey questions, stratified by transferring hospital.To complement this quantitative analysis, we conducted nine User-Centered Design (UCD) sessions between 2/2023-7/2023 involving 22 clinicians who interact with the EHR during IHT including 3 medicine residents, 10 advanced practice providers, 5 direct care attendings, and 4 Access Center nurses responsible for triaging all IHTs. UCD sessions utilized guided discussions to gather input on EHR workflow during IHT patient admission, including barriers to data access and availability. UCD sessions were recorded, analyzed, and coded by two independent reviewers (JK and PG) to identify themes.
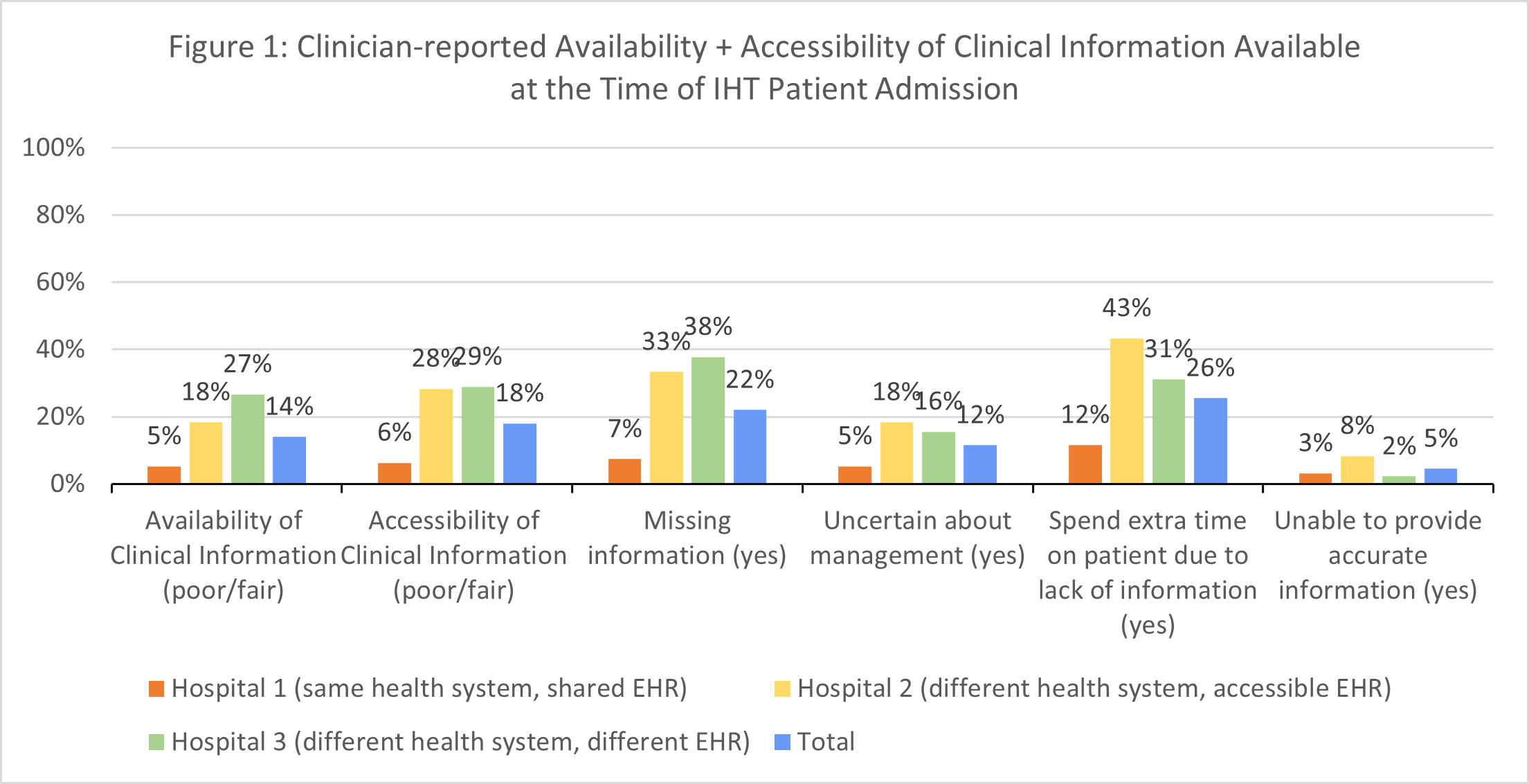
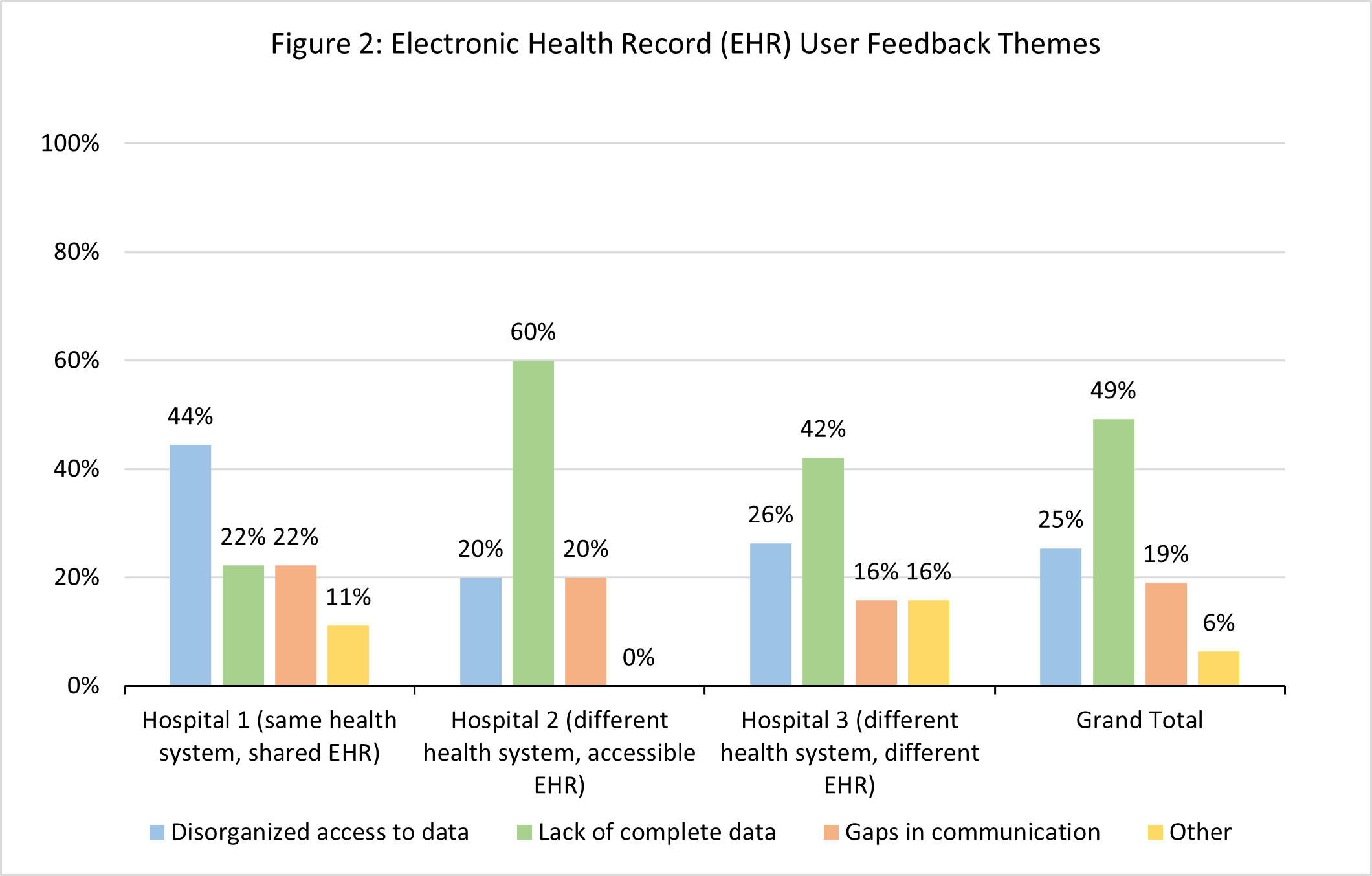
Results: Of the 328 IHT patients included, we received 200 clinician survey responses (61% response rate) including 95 from Hospital 1, 60 from Hospital 2, and 45 from Hospital 3. Responses stratified by transferring hospital are shown in Figure 1.Analyses of the UCD sessions identified 3 major themes related to data access and availability during IHT including: (1) lack of access to complete data, (2) data organization and navigation issues and (3) gaps in communication. Distribution of themes by transferring hospital is shown in Figure 2.
Conclusions: Among front-line clinicians who manage IHT to a large tertiary care center, we found that a significant number of clinicians experience suboptimal availability of clinical information available in the EHR at time of IHT and high reported rates of missing information and inefficient care management, particularly among IHT from Hospitals 2 and 3 (different healthcare systems). Qualitative evaluation supports these findings and shows disproportionate reports of disorganized data among IHT from Hospital 1, and disproportionate reports of lack of complete data among IHT from Hospitals 2 and 3. These data provide valuable targets that we will leverage to improve access to and accessibility of clinical data at time of IHT.