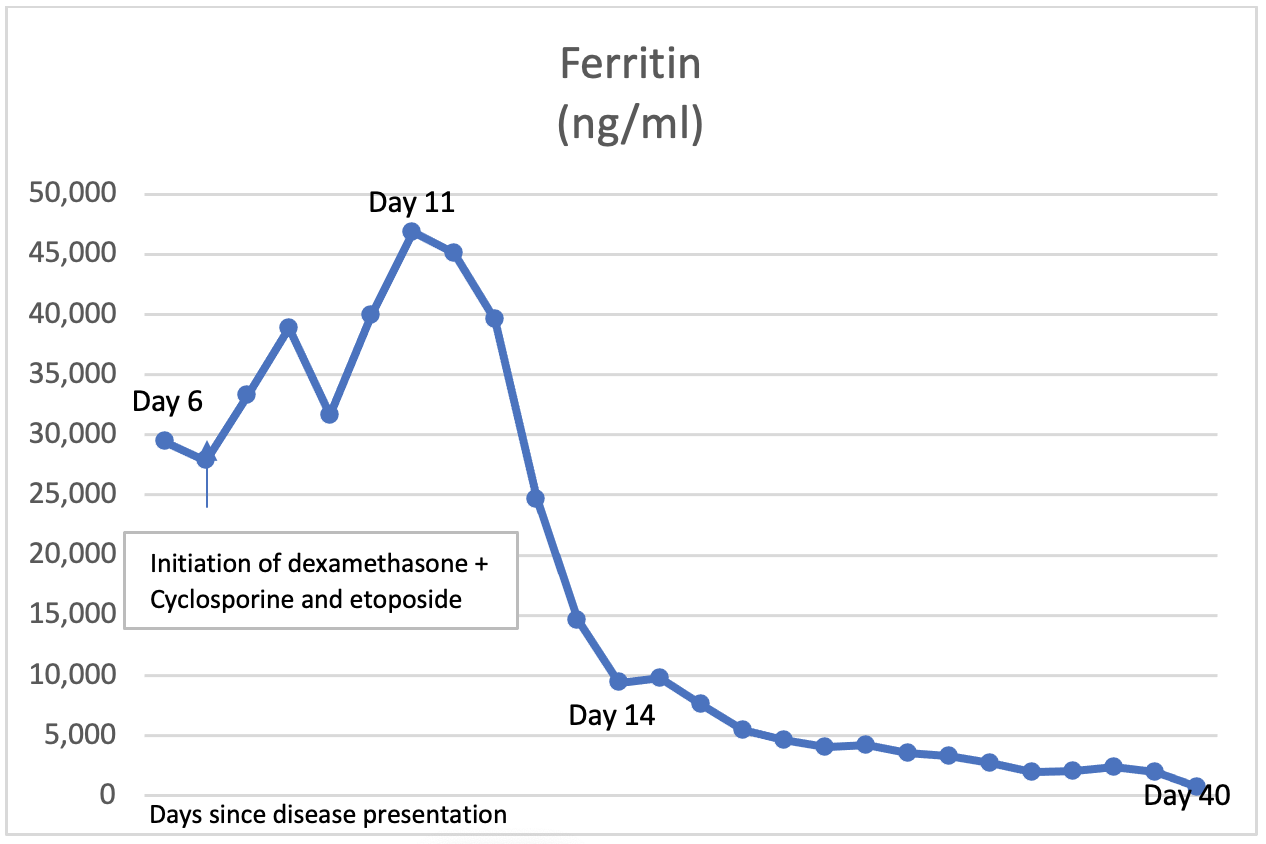
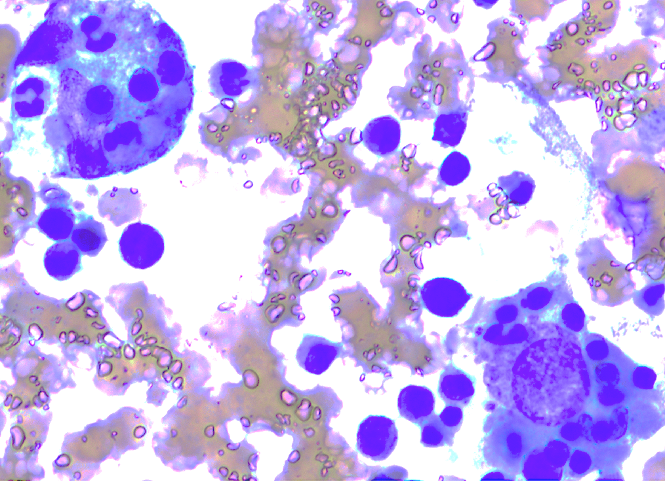
Case Presentation: A 27-year-old female without any significant medical history, who developed acute kidney injury, metabolic acidosis, increasing liver enzymes, coagulopathy, anemia, thrombocytopenia and undifferentiated shock requiring pressors on 6th post-partum delivery. Peripheral smear showed atypical lymphocytes, dohle bodies and neutrophils with toxic vacuolization, suggesting an inflammatory processOther labs were significant for elevated ferritin levels that peaked at 46,812 ng/mL, elevated IL-2, elevated triglycerides The bone marrow biopsy showed normocellular marrow with numerous histiocytes and frequent hemophagocytosis , which confirmed the diagnosis of HLH. She was treated with HLH 2004 protocol which includes etoposide, cyclosporine (CSA) and dexamethasone. The immediate post treatment course was encephalopathy and generalized seizures requiring mechanical intubation. MRI of the brain showed multiple areas of hyperintensity without diffusion restriction in the cortical/subcortical distortion in the supratentorial and infratentorial brain, consistent with Posterior reversible encephalopathy syndrome (PRES). The etiology of PRES was debatable between secondary to cyclosporine and/or HLH. CSA was held for two weeks due to concerns that it could potentiate PRES. The workup to determine infectious, rheumatological, malignant and familial etiology was unremarkable. The patient’s clinical condition improved rapidly, she was extubated after 7 of starting treatment and was discharged on treatment day 21 to continue protocol as outpatient. The patient has received 8 weeks of HLH 2004 protocol including intrathecal treatment and has continued to demonstrate improvement in clinical and laboratory parameters.
Discussion: Hemophagocytic lymphohistiocytosis (HLH) is an aggressive immune activation syndrome with high mortality without early identification and treatment. In adults, most HLH are secondary rather than genetic, as in pediatrics. Early recognition is paramount and treatment of the underlying disease along with controlling immune dysregulation is the key to improve disease outcomes. Commonly reported cases are secondary to infection, rheumatologic disorder and malignancies. Here we report a case of 27-year-old female who developed HLH postpartum without other clear inciting cause.
Conclusions: Post-partum HLH is a rare and fatal immune activation syndrome with limited available literature. During postpartum period, while there is gradual reversal of maternal pregnancy-related physiological change, the T cell immunomodulation and suppression of NK cytotoxicity may persist leading to the development of HLH. Patients with CNS involvement have adverse prognosis and increased awareness of HLH in the postpartum is necessary for prompt diagnosis and treatment initiation is the key for improved outcomes.