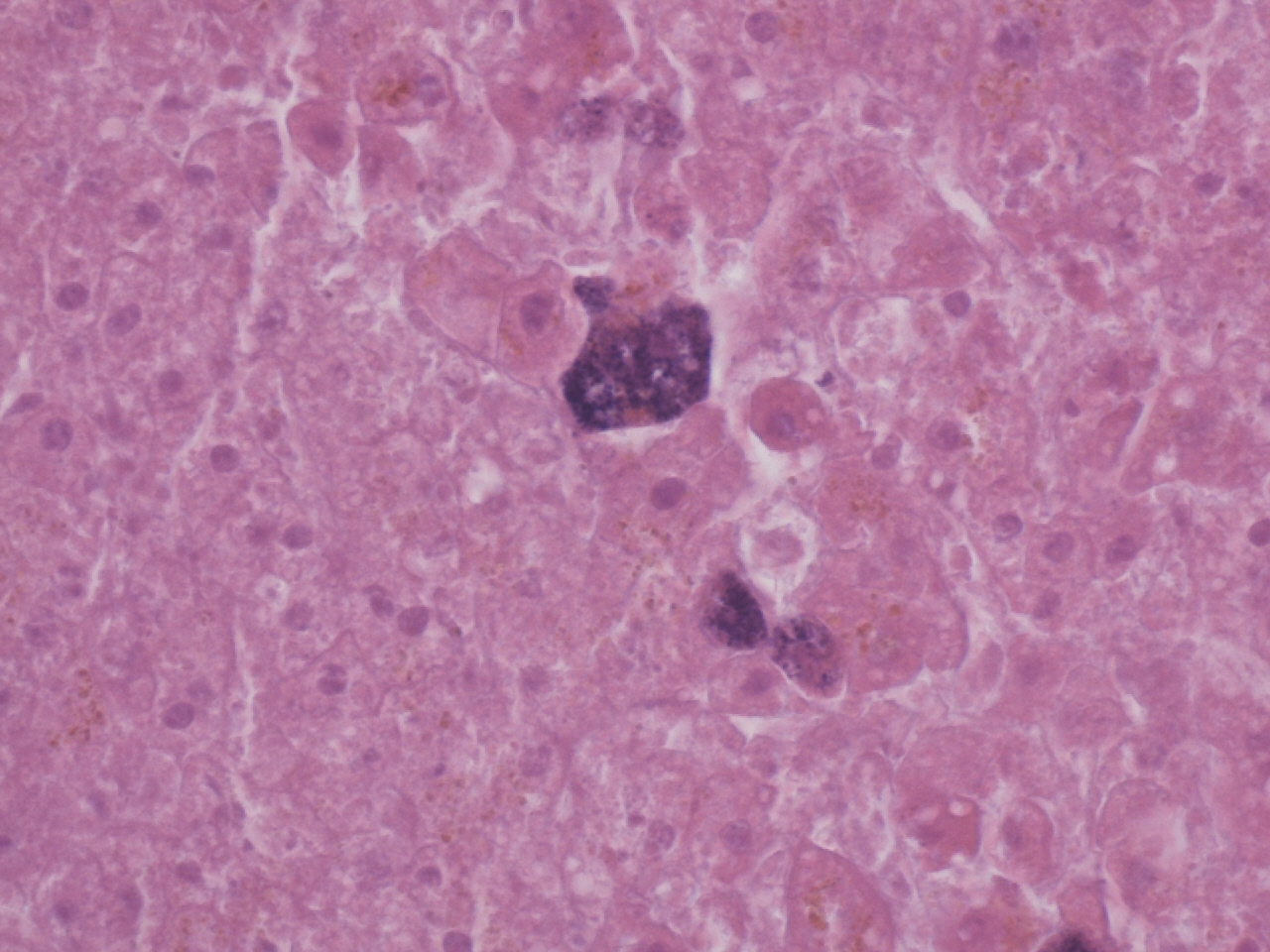
Case Presentation: We present the case of a 41 yr old man who was admitted for acute renal failure and initially presented with myalgias, anuria, and shortness of breath. Upon admission, the patient was initially febrile to 103.1 F and tachycardic to HR 126/minute. A Quinton catheter was placed for dialysis initiation. Infectious Disease was consulted for persistent fevers >103 F. CT abdomen was notable for enteritis and CT chest revealed mediastinal lymphadenopathy and a small loculated pleural effusion. He underwent a thoracentesis and pleural studies were negative for infection. Cefazolin and metronidazole were initiated, but no significant improvement was noted in fever or leukocytosis. No focal source of infection was seen on tagged WBC scan or echocardiogram and blood cultures remained negative. His fever persisted and antibiotics were broadened to piperacillin/tazobactam. Hematology/oncology was consulted for suspicion of HLH (ferritin >10,000) and for suspected hematologic malignancy being the cause for his recurrent fevers. The dialysis line was removed, but the patient became encephalopathic and exhibited mild aphasia. CT head and MRI brain were unremarkable at that time. Antibiotics were adjusted to vancomycin and ceftriaxone for suspected meningitis. Initial lumbar puncture was unsuccessful and plans were made to perform lumbar puncture by Interventional Radiology. This patient underwent PEA arrest, ROSC was achieved, he was transferred to the ICU requiring 3 pressure for shock. Repeat CT abdomen revealed a fluid collection involving the left psoas, suspected to be an abscess. He sustained a second PEA arrest later that day with transient ROSC and then progressed back to PEA arrest again shortly after and expired. Autopsy findings revealed disseminated Toxoplasma infection as well as evidence of cytophagocytosis present in the lymph nodes. There was hemorrhage present in the left psoas muscle that was presumed to be spontaneous due to hypocoagulable state. The etiology of his mental status changes was most likely due to Toxoplasma encephalitis and his autopsy was also significant for Toxoplasma myocarditis and hepatitis.
Discussion: Disseminated toxoplasmosis (DT) is a rare, life-threatening infection that affects predominantly immunocompromised hosts. It is defined by the presence of Toxoplasma gondii cysts or tachyzoites in more than one organ or in the blood. Haemophagocytic lymphohistiocytosis (HLH) is a severe and potentially fatal hyperinflammatory syndrome. Infection-associated HLH is caused by pathogens, most commonly Epstein-Barr virus, Cytomegalovirus, HIV, mycobacteria, and endemic fungi. Only a few cases of DT in immunocompetent individuals have been reported and its association with HLH is rarely seen.
Conclusions: HLH associated with DT is rare, difficult to diagnose, and can lead to poor prognosis without early and aggressive treatment. It is crucial to confirm the presence of HLH based on the HLH-2004 criteria and HScore and identify and treat the causative organism, as uncontrolled infection can lead to HLH. It is important to consider dissemination of toxoplasmosis even in immunocompetent individuals.