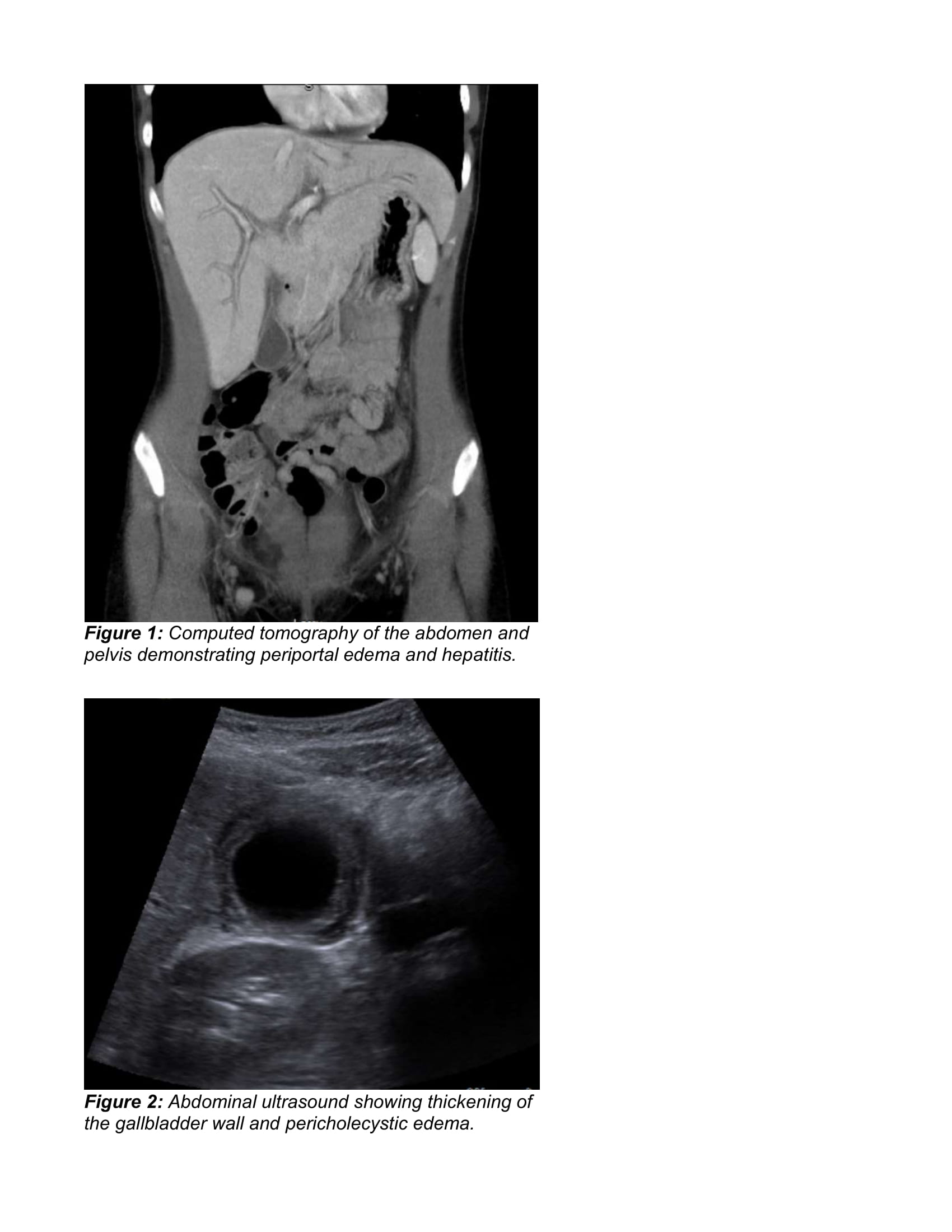
Case Presentation: A 17-year-old female with no past medical history was admitted to a tertiary care children’s hospital with acute onset of abdominal pain, nausea, emesis, oral ulcers, and vaginal rash. She was sexually active with the last unprotected encounter nine days prior to presentation. She endorsed dysuria but denied vaginal discharge. The patient was afebrile with normal vital signs, ill-appearing, and pale. HEENT exam was notable for palatal vesicular lesions and tender cervical lymphadenopathy. Abdominal exam showed diffuse tenderness without rebound or guarding. Genitourinary exam revealed vulvar vesicular lesions. On diagnostic evaluation, initial labs showed hypokalemia and mild leukocytosis. The oral and genital lesions were positive for HSV-1. Gonorrhea and chlamydia testing, HIV 1/2, syphilis, hepatitis panel, UA, urine culture, hCG, and rapid flu were negative. CT abdomen/pelvis showed nonspecific periportal edema and abdominal ultrasound showed a thickened gallbladder wall, hyperemia, and pericholecystic fluid. HIDA scan was normal. Pelvic ultrasound showed no ovarian torsion. Chest x-ray was unremarkable. Brain MRI, lumbar puncture, and EEG were obtained due to severe headache with associated nausea and photophobia and were normal. Subsequent labs included a positive serum HSV-1 PCR. EBV panel had positive IgM, IgG, and EBNA, but negative early antigen. These results with a negative monospot were consistent with reactivation or recovery. Serial CMPs showed elevated AST (137) and ALT (165), which normalized over four days. ESR, CRP, amylase, and lipase were normal. HSV and EBV PCRs were negative after symptoms improved.
Discussion: The patient was diagnosed with primary HSV infection including HSV-1 viremia and oral and genital lesions. She had concomitant reactivation of EBV. The periportal edema on abdominal CT with acute transaminitis, abdominal pain, and emesis supported the diagnosis of acute hepatitis. Gallbladder inflammation on ultrasound with normal function on HIDA scan was also consistent with hepatitis rather than cholecystitis. While PID was initially considered, she had negative STI testing and no symptomatic improvement on antibiotics, so these were discontinued.
Conclusions: This adolescent female had symptoms of acute hepatitis with disseminated HSV-1 and reactivated EBV. Disseminated HSV has been associated with hepatitis, but most commonly occurs in immunocompromised, neonatal, or pregnant patients rather than adolescents. Most cases of HSV hepatitis present as fulminant disease with high mortality rates, but better outcomes including spontaneous recovery have been reported in children compared to adults. Our patient’s presentation was uniquely mild to moderate in severity, which can also be attributed to early diagnosis and treatment with IV acyclovir. Ultimately, her symptoms improved on a 10-day course of IV acyclovir during the 2-week hospitalization.