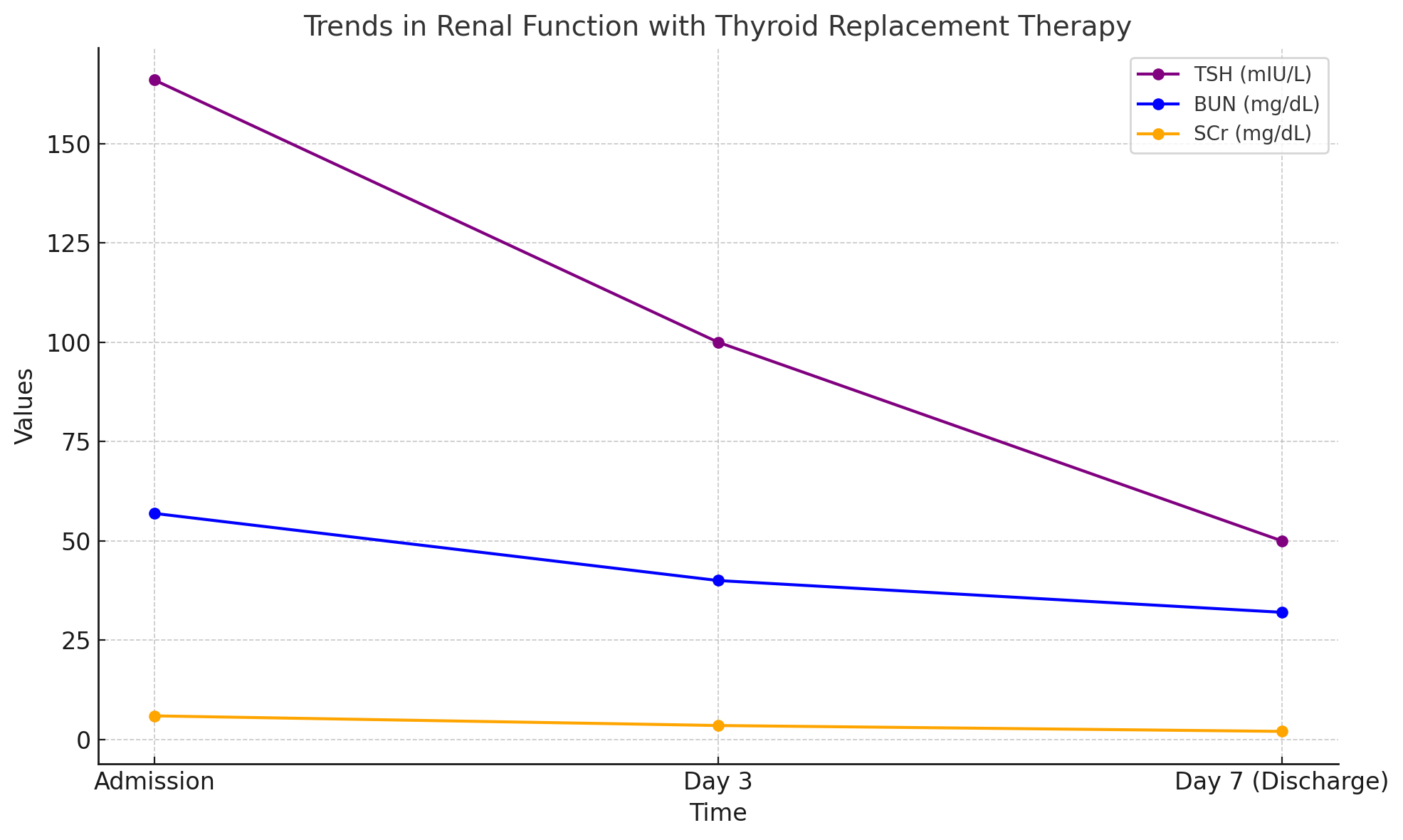
Case Presentation: A 77-year-old male with history of hypertension, hyperlipidemia, type 2 diabetes mellitus, and chronic kidney disease (stage 3a) presented with generalized weakness and fatigue. He denied other symptoms, including myalgias, cold intolerance, or oliguria. Laboratory evaluation revealed blood urea nitrogen (BUN) of 56.9 mg/dL, serum creatinine (SCr) of 5.93 mg/dL, and glomerular filtration rate (GFR) of 12 mL/min/1.73 m², consistent with acute kidney injury (AKI) on chronic kidney disease (CKD). Thyroid function tests showed profound hypothyroidism with thyroid-stimulating hormone (TSH) of 166 mIU/L, free T4 of 0.13 ng/dL, and total T3 of 1.07 ng/mL. Creatine kinase was normal. Renal ultrasound showed no obstruction, and no nephrotoxic medications were identified. The patient was started on levothyroxine 50 mcg daily for thyroid hormone replacement. Following several days of thyroid supplementation, renal function improved significantly and returned to his baseline, with discharge labs showing BUN 32 mg/dL, SCr 2.02 mg/dL, and GFR 38 mL/min/1.73 m². The patient was discharged with appropriate outpatient follow up.
Discussion: Hypothyroidism is a rarely reported cause of acute kidney injury (AKI). Thyroid hormones play a crucial role in maintaining renal hemodynamics, influencing glomerular filtration rates and tubular reabsorption. Manifestations of hypothyroidism can be subtle; therefore, a high index of suspicion is needed in case of unexplained kidney dysfunction, particularly in hospitalized patients with complex conditions that may obscure the diagnosis. In our case, a patient with chronic kidney disease developed acute kidney injury in the setting of severe, untreated hypothyroidism. The marked improvement in renal function following thyroid hormone replacement strongly supports hypothyroidism-induced nephropathy as the likely etiology.
Conclusions: Hypothyroidism should be considered in the differential diagnosis of unexplained AKI, particularly in patients with significant thyroid dysfunction. Prompt identification and treatment can lead to substantial renal recovery, as demonstrated in this case.