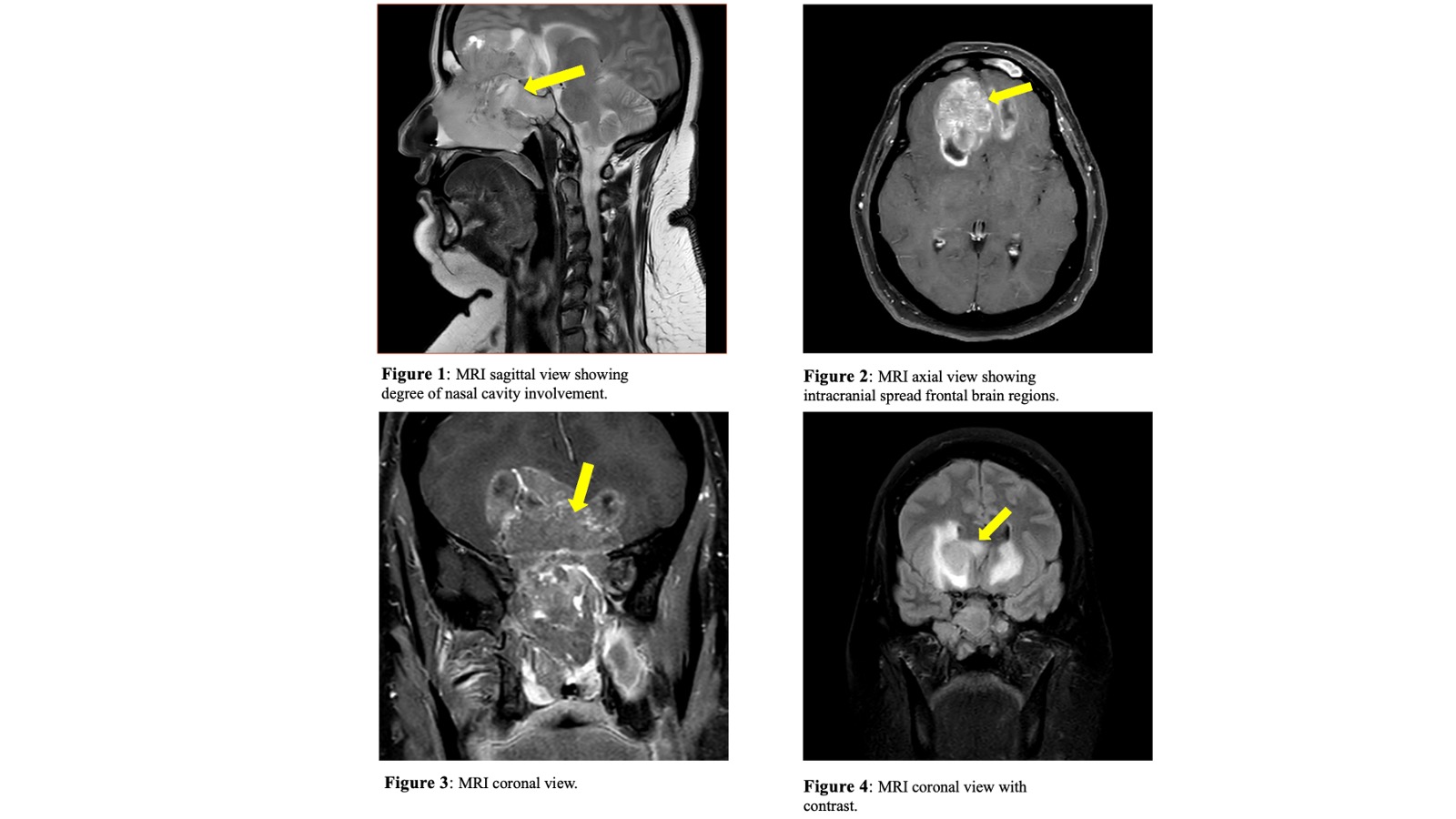
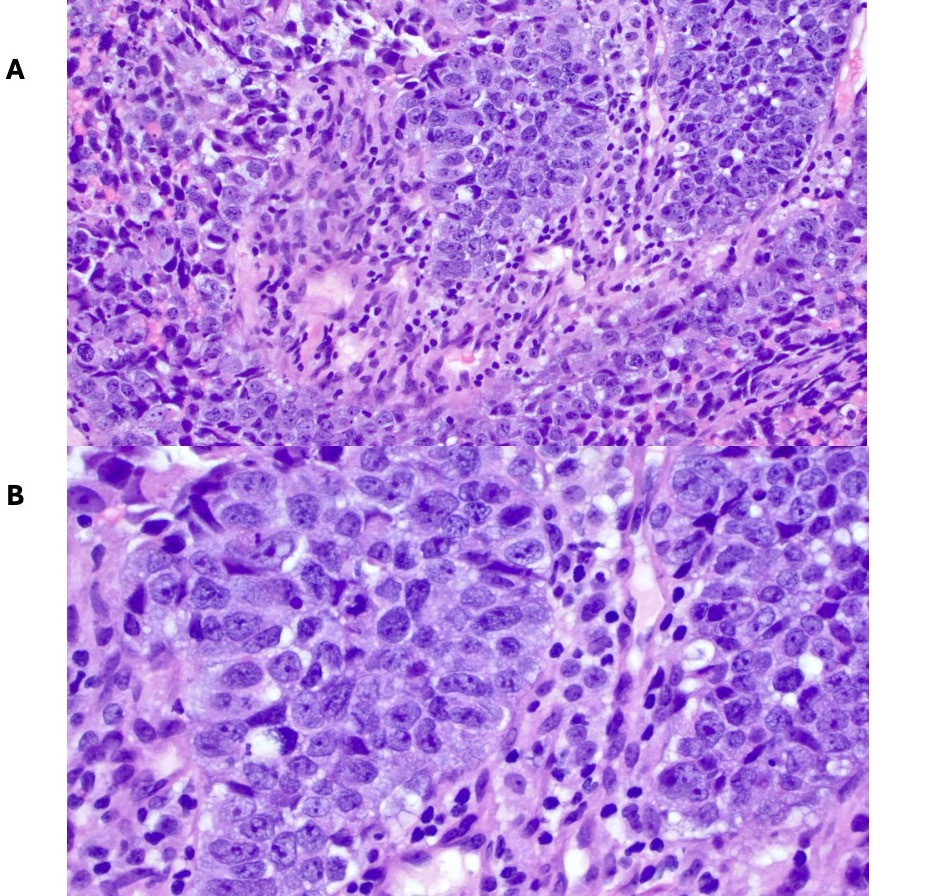
Case Presentation: A 51-year-old female with a BRCA mutation and a history of prophylactic bilateral mastectomy presented with neuropsychiatric symptoms, including confusion, memory loss, and excessive sleep. Her medical history included hysterectomy and parotid tumor resection and a family history of various cancers, including prostate, lung, and lymphoma. Initial symptoms, including headaches and nasal congestion, were treated as bacterial sinusitis. Persistent symptoms despite antibiotic treatment led to imaging, revealing an invasive mass in the nasal cavity extending into the frontal lobes. Nasal endoscopy and biopsy confirmed large cell neuroendocrine carcinoma (LCNEC) with immunohistochemical positivity for CKA1/3, CD56, synaptophysin, and CK5/6. Metastatic workup showed no distant disease. The tumor’s extensive involvement of critical structures required a collaborative surgical plan with neurosurgery and ENT skull base specialists.
Discussion: Sinonasal neuroendocrine tumors represent approximately 1% of sinonasal malignancies, with LCNEC being particularly rare. There are only 12 documented cases in the scientific literature. The patient’s symptoms, initially mistaken for sinusitis, illustrate how sinonasal LCNEC can resemble benign conditions. Though distant disease was absent, the tumor’s extensive local spread complicated surgical planning, necessitating a multidisciplinary approach. Standard treatment for sinonasal LCNEC, a poorly differentiated, locally invasive tumor, generally includes surgery, radiation, and chemotherapy; however, outcomes are often poor due to the tumor’s aggressive behavior. This case emphasizes the importance of thorough assessment, especially in patients with genetic predispositions to cancer, to allow timely diagnosis and intervention.
Conclusions: This case of sinonasal LCNEC with brain extension in a patient with a significant family cancer history highlights challenges in diagnosing and treating rare neuroendocrine malignancies. Delayed diagnosis due to benign-like symptoms emphasizes the need for thorough evaluations in high-risk individuals. Successful management in this case was achieved through coordinated efforts between neurosurgery and ENT. Future research on the molecular basis of LCNEC and standardized treatment protocols is crucial to improve outcomes. Emphasizing long-term follow-up is essential due to high recurrence and metastasis risks.