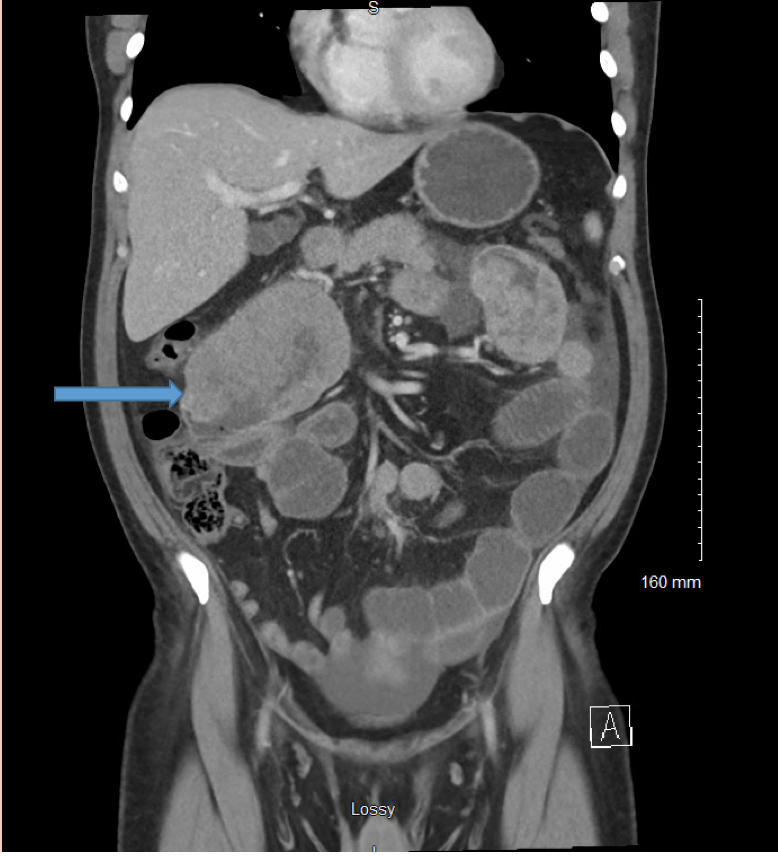
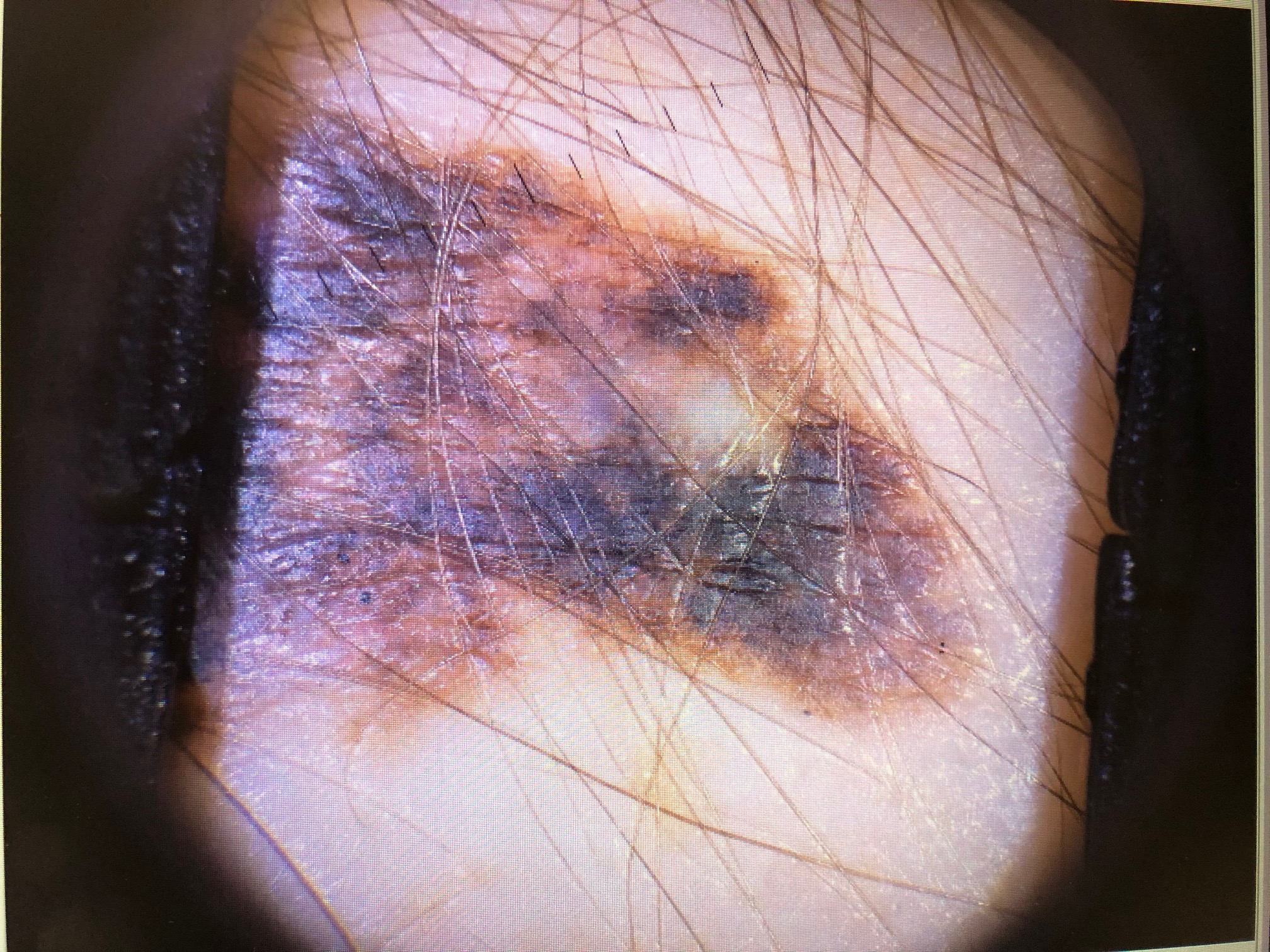
Case Presentation: 47-year-old male veteran presented with one-month history of intermittent left-sided abdominal pain, vomiting, constipation and melena. Abdominal X-ray revealed small bowel obstruction. CT scan of the abdomen and pelvis with contrast revealed multifocal masses involving proximal to mid-small bowel with small bowel obstruction secondary to the mass at the level of jejunal and ileal junction. Dominant mass in the right mid abdomen was measured at 11.5 cm. There were additional central abdominal and pelvic mesenteric adenopathy with evidence of early nodal necrosis. The patient underwent exploratory laparotomy with small bowel resection and colectomy with anastomosis. The biopsy was positive for malignant melanoma (BRAF negative). On the day of surgery, further physical examination showed a large lesion with irregular border and texture on the left scapula. Biopsy of the lesion revealed malignant melanoma. PET scan showed multiple enlarged and hypermetabolic metastatic lymph nodes in the abdominal mesentery and to a lesser extent in the left axilla. The patient was scheduled to receive ipilimumab and nivolumab.
Discussion: The above clinical scenario depicts a rare occasion wherein malignant melanoma presents initially as an intestinal obstruction rather than as a skin lesion. According to the published literature, even in patients with primary cutaneous melanoma, symptomatic gastrointestinal metastases are rare and is more likely an autopsy finding.Malignant melanoma is the fifth most common cancer and the most aggressive form of skin cancer. Melanoma can arise from melanocytes in the skin (most common) or melanocytes in the mucosal epithelium lining the respiratory, gastrointestinal and genitourinary tracts. Mucosal melanomas are rare and carry a worse prognosis.Risk factors for malignant melanoma include age >60 years, male sex, atypical moles, squamous or basal cell carcinoma, immunosuppression, melanoma susceptibility polymorphisms, ultraviolet light exposure from sunlight and use of tanning beds. This patient is a veteran and had chronic sun exposure from his line of duty as military personnel in the past. According to a systematic review of nine published studies on melanoma and non-melanoma skin cancer in military personnel in the United States, melanoma risk is increased in military service, especially in the Air Force personnel, compared to the general population. It was implicated to be due to increased sun exposure, low rates of routine sunscreen use and inadequate patient education and screening protocols.The most common acquired gene mutation is in BRAF oncogene, seen in about half of all melanomas. In mucosal melanomas (melanomas occurring in parts of the body that are rarely exposed to sunlight), mutations are noted in C-KIT gene. Treatment options in advanced melanoma include targeted therapy (BRAF inhibitors), immunotherapy (also called checkpoint inhibitor therapy), chemotherapy, surgery and radiation for symptomatic metastases. Targeted therapy with BRAF inhibitors is not helpful for this patient as biopsy was negative for BRAF mutation, so immunotherapy with PD-1 inhibitors (Nivolumab) and CTLA-4 inhibitors (Ipilimumab) was given to our patient.
Conclusions: Malignant melanoma should be considered as a differential diagnosis in a patient with mechanical small bowel obstruction and should warrant a thorough search for skin melanoma. People with risk factors for melanoma should be encouraged to get regular skin inspections for early detection of melanoma.