Background: Acute decompensated heart failure exacerbation is the leading cause of hospitalization in the United States. It was associated with total medical costs of more than $30 billion in 2012 with projections estimating around $70 billion in costs by 2030. Currently, six million people in the U.S. have heart failure, with a little over half a million new cases diagnosed annually. Administration of loop diuretics is the cornerstone of inpatient management. Previous studies such as the DOSE trial compared outcomes for different dosing strategies; however, the optimal goal for daily fluid balance is not known. Using the MIMIC-III database, an openly available dataset of de-identified health data on intensive care unit (ICU) admissions, we compared outcomes for higher versus lower daily net negative fluid balance in adults admitted for acute decompensated heart failure.
Methods: The Medical Information Mart for Intensive Care (MIMIC-III) database was used to identify patients admitted to the ICU for a heart failure exacerbation. Patients had to have a heart failure diagnosis using International Classification of Diseases, 9th edition codes and must have been administered at least one dose of parenteral diuretics within their first 24 hours of ICU admission. Only a patient’s first ICU admission was evaluated. Patients who were neonates (age <1 year), had a serum creatinine >3 mg/dL at ICU admission, or had an ICU admission <12 hours were excluded. Maximum 24-hour negative fluid balance within the first 72 hours of ICU admission was calculated for each patient. Patients were classified into high- or low-intensity diuresis groups if the negative fluid balance was greater than 3000 ml or less than 3000 ml respectively. The primary outcome was the difference in ICU length of stay (LOS) between diuresis groups. Secondary outcomes included SCr and an a priori Oxford Acute Severity of Illness Scores (OASIS) score subgroup analysis for the primary outcome.
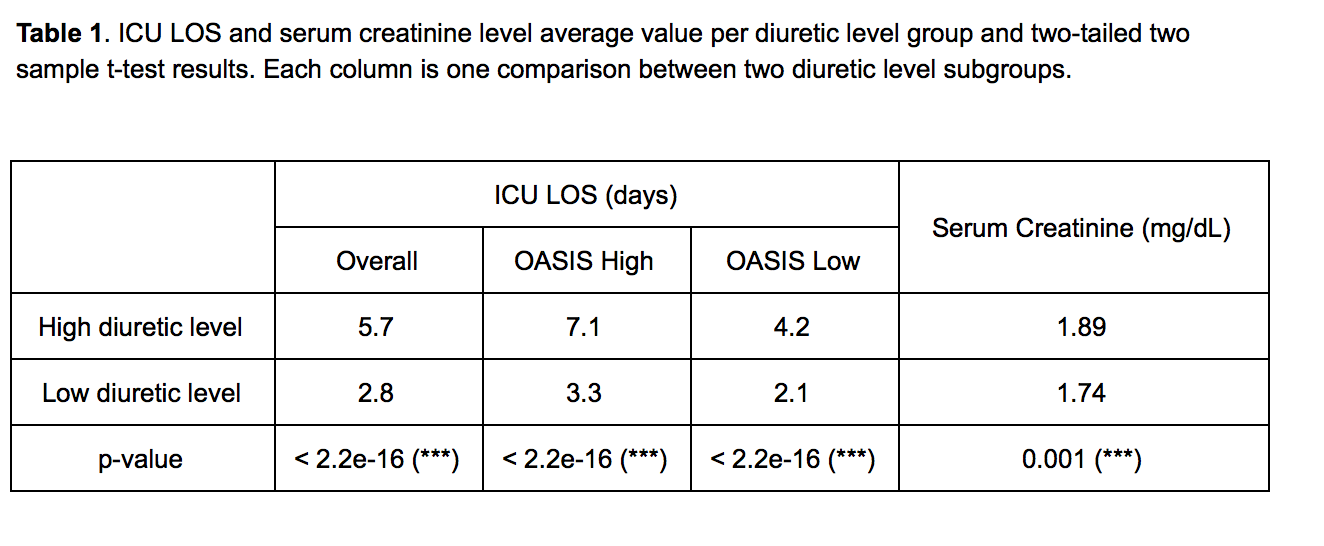
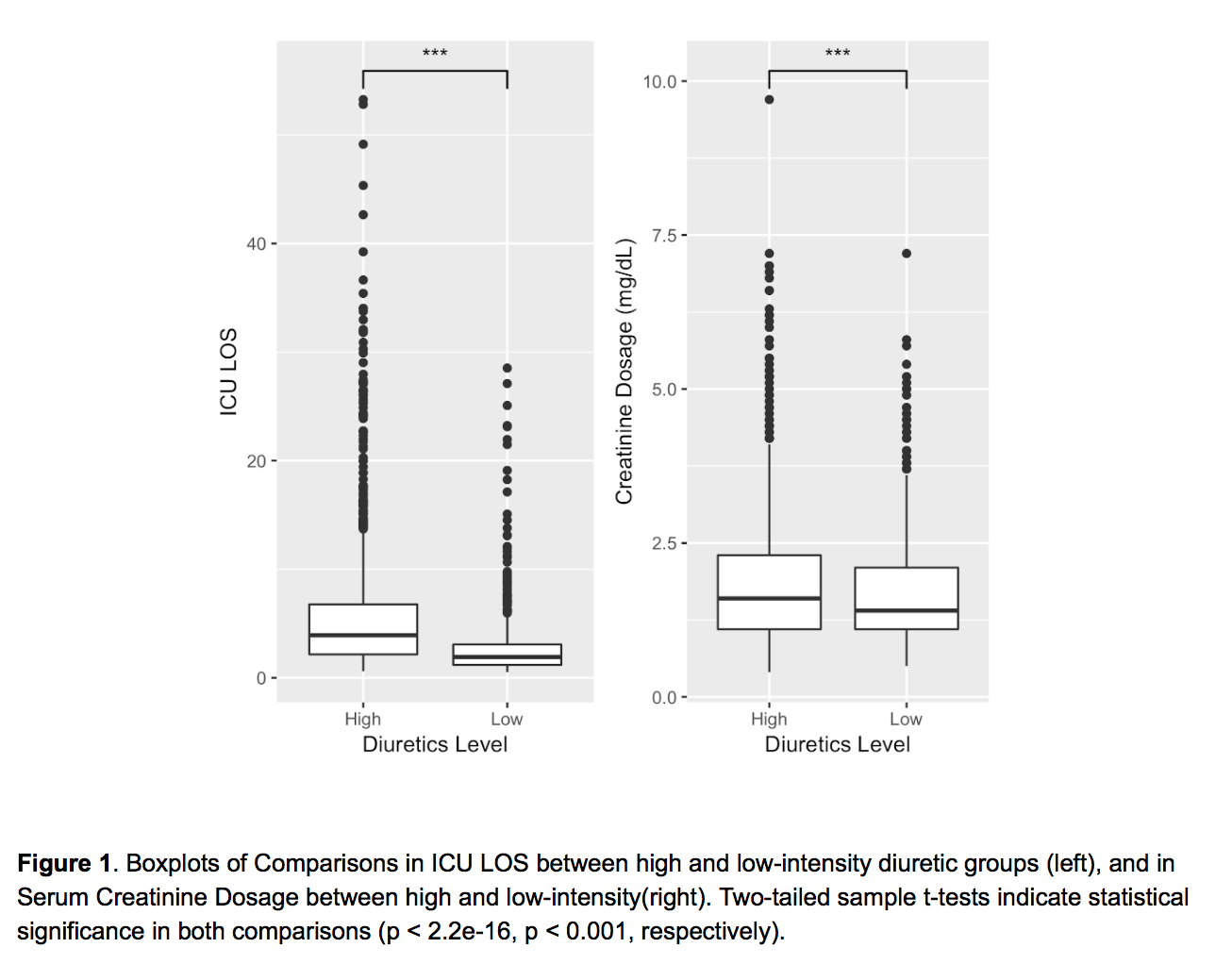
Results: A total of 46,520 patients were screened for inclusion/exclusion criteria, of which 4,031 patients were included in this study. Two-tailed two sample t-tests showed a statistically significant increase in ICU LOS (p-value < 2.2e-16) and serum creatinine level (p = 0.001) in high- versus low-intensity diuresis groups (Figure 1). ICU LOS remained significantly different between high- and low-intensity diuresis groups stratified by OASIS score (Table 1).
Conclusions: Increased diuresis (more negative fluid balance) was correlated with longer ICU stay. This association remained even when patients were stratified by disease severity. On further examination, increased diuresis was associated with higher creatinine level, suggesting that acute kidney injury may be one possible driver for the longer length of stay. Future steps include prospective analyses comparing different diuretic goals.