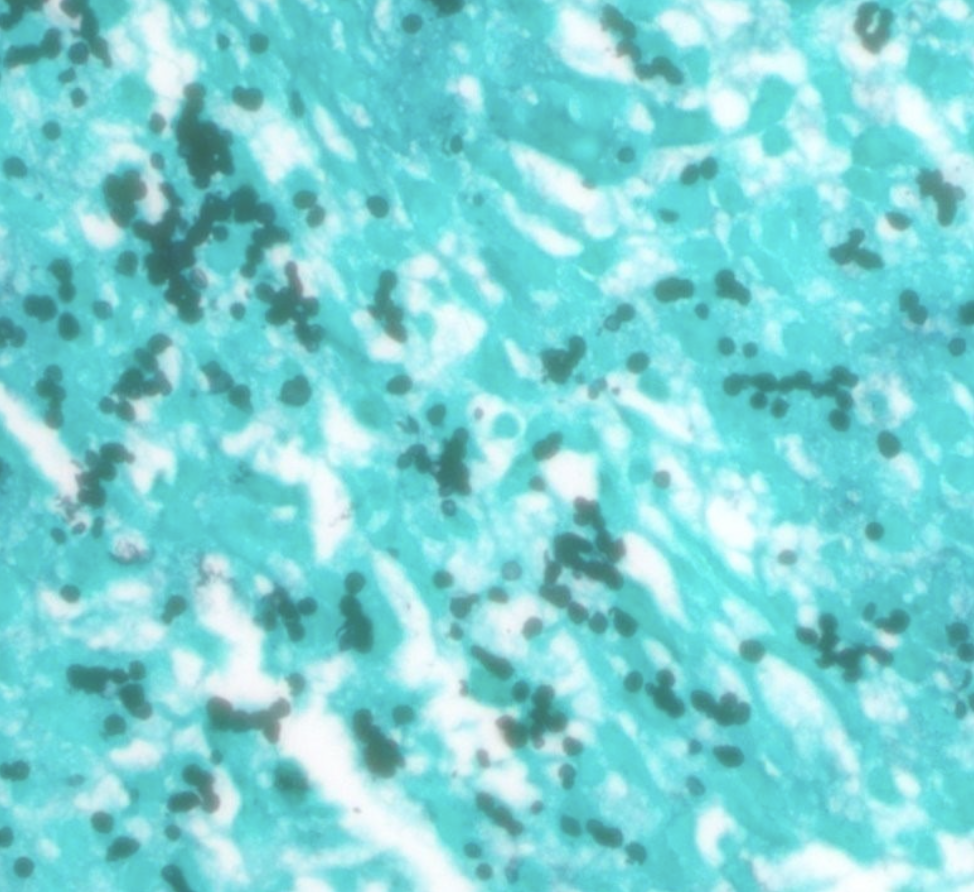
Case Presentation: A 33-year-old female with a renal transplant 18 months prior was transferred to our hospital with acute kidney injury after presenting with acute gastrointestinal symptoms. One year earlier, a biopsy of the transplanted kidney revealed budding yeast consistent with Histoplasma capsulatum. Histoplasma urine and serum antigens were negative, and Itraconazole was discontinued after three days due to gastrointestinal side effects. No further treatment was pursued as subsequent antigen tests were negative. At presentation, workup for common infectious etiologies were negative except for elevated quantitative plasma CMV by PCR. Symptoms persisted on empiric antibiotics, and she developed fevers and hematochezia. Colonoscopy showed discontinuous ulcers and further testing revealed positive urine Histoplasma antigen (Figure 1). Grocott’s methenamine silver (GMS) stain of colon biopsy showed spore-forming organisms morphologically compatible with Histoplasma capsulatum (Figure 2). Itraconazole was started and symptoms significantly improved within two days.
Discussion: Histoplasmosis is the most common endemic mycotic infection in solid organ transplant (SOT) patients, though it is rare, with a 1-year incidence of 0.1% [1, 2, 3]. Disseminated disease occurs in the majority of these cases [1, 3]. Symptomatic gastrointestinal histoplasmosis (GIH), as seen in this case, is uncommon, occurring in only 3-12% of disseminated histoplasmosis (DH) cases [3, 4]. The overlap of GIH symptoms with more common gastrointestinal diseases can lead to delayed diagnosis. The gold standard for diagnosing GIH is tissue sampling and fungal cultures, but diagnosis is often made by staining and microscopy [5]. Periodic Acid-Schiff or GMS stains offer better visualization of Histoplasma than hematoxylin and eosin [5]. In this case, initial pathological investigations did not include GMS or PAS staining; these were requested after an elevated urine Histoplasma antigen result. Given the ease of obtaining urine and serum antigens, it is important to consider their early inclusion in the infectious workup in cases such as this one [6]. Treatment guidelines for GIH recommend at least 12 months of therapy with itraconazole, with or without an initial 2-week course of Amphotericin B depending on the severity of symptoms [3]. Regular monitoring of urine or serum antigen levels is advised [5]. Although antigen levels may remain detectable but low in SOT patients, treatment can be discontinued after completing the full course [3, 6, 7].
Conclusions: This case highlights a rare presentation of GIH in SOT. It underscores the importance of a broad differential diagnosis and considering Histoplasma as an infectious etiology in immunocompromised patients presenting with gastrointestinal symptoms, particularly those with a history of histoplasmosis. Prompt testing for Histoplasma antigens or appropriate tissue staining is crucial for timely diagnosis and treatment.