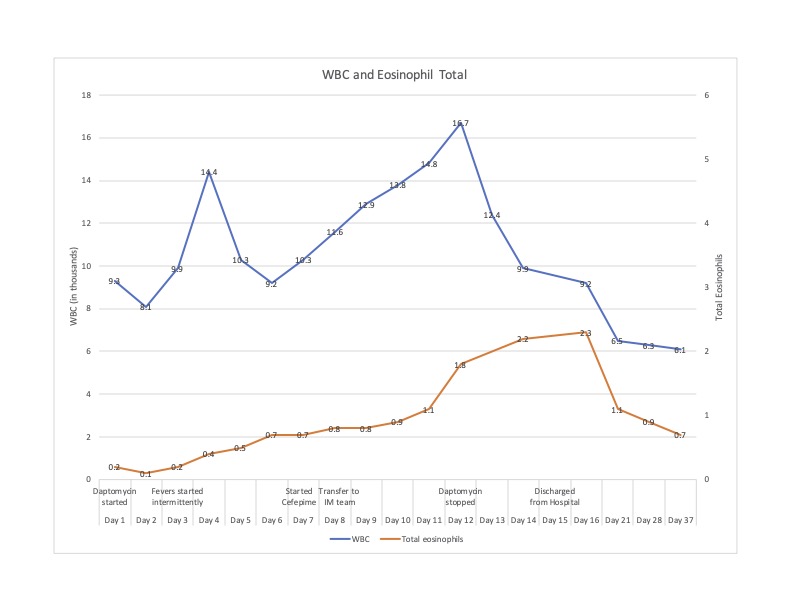
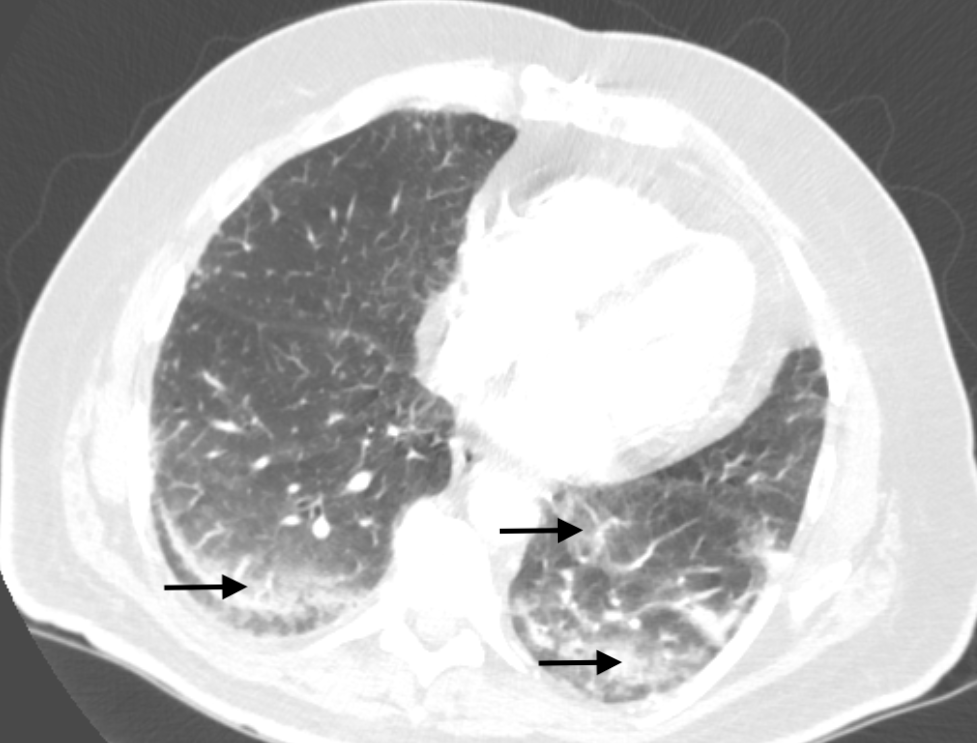
Case Presentation: A 68-year-old patient with history of type 2 diabetes (A1c 9.5%) was admitted to the podiatry service following a partial fifth ray resection for osteomyelitis. Bone cultures grew MRSA and ID recommended 6 weeks of IV daptomycin due to an allergy to vancomycin. His post-op course was complicated by multiple days of recurrent fevers, dyspnea, and hypoxia. CTA of the chest revealed bilateral ground-glass opacities with increasing consolidation in the lower lobes concerning for hospital-acquired pneumonia. He was started on cefepime and transferred to the internal medicine service. At the time of transfer, O2 saturation was 92% on 2L NC, and exam was notable for bilateral lower lobe crackles. Labs were significant for a WBC count of 11.6 10³/µL with 67% PMNs, 17% lymphocytes and 7% eosinophils, with an absolute eosinophil count of 0.8 10³/µL. Blood cultures, sputum culture, COVID-19, respiratory viral panel, and legionella urinary antigen all returned negative. After transfer, he had persistent oxygen requirements, daily spiking fevers, and rising WBC count. Podiatry reported good source control and no evidence of surgical site infection, blood cultures remained negative, and TTE showed no evidence of endocarditis. The case was again reviewed with ID, and it was noted that the absolute eosinophil count was rising dramatically. Given concern for daptomycin-induced acute eosinophilic pneumonia, daptomycin was stopped, and pulmonology was consulted. They found documentation from 15 years prior when the patient had a similar respiratory illness and eosinophilia while on daptomycin. They considered BAL for diagnostic purposes but opted to avoid the procedure, citing that the clinical picture and prior episode were sufficient to make a probable diagnosis of daptomycin-induced acute eosinophilic pneumonia. After stopping daptomycin, the patient defervesced and his dyspnea resolved. Steroids were considered but ultimately deferred given his rapid clinical improvement. He was discharged on PO linezolid and his WBC and eosinophil count normalized within 3 weeks of discharge.
Discussion: This case meets criteria for a probable diagnosis of daptomycin-induced acute eosinophilic pneumonia per guidelines from the FDA. Definite diagnosis requires BAL which was deferred (1). Our patient resembles many described in the literature. One systematic review of 35 reported cases found that 83% of patients were male with median age 65.4 +/- 15 years (2). Most patients had dyspnea (94%), peripheral eosinophilia (77%), infiltrates on lung imaging (86%), and fever (57%). Typical lab findings include initial neutrophilic leukocytosis without eosinophilia followed by a rise in eosinophil count as the disease progresses. The most common reason for daptomycin use was osteomyelitis (2). In another review, the mean time to diagnosis after symptom onset was 9.8 days, demonstrating the diagnostic dilemma presented by this entity (3). Treatment includes stopping daptomycin and often includes steroids, although there is no agreed upon standard of care. In this case, the patient improved upon discontinuation of daptomycin and the risks of steroids were thought to outweigh the benefits.
Conclusions: Clinicians should consider eosinophilic pneumonia as a cause of fevers and/or respiratory decompensation in patients receiving daptomycin. Swift diagnosis and discontinuation of daptomycin can lead to clinical recovery even without the administration of steroids.