Background:
Clostridium difficile infection (CDI) is a growing epidemic in U.S. hospitals. Much of the rapid rise in severe cases of CDI over the past 10 years is thought to be from the fluoroquinolone (FQ)–resistant strain of bacteria BI/NAP1/027. Reducing patient exposure to FQ is a key strategy in reducing CDI. It is unclear which strategies are superior in appropriately reducing FQ administration in community hospitals. Hospitalists are increasingly expected to optimize delivery of pharmacotherapy to inpatients. We studied the effects of a program educating and reminding hospitalists of ideal FQ use.
Methods:
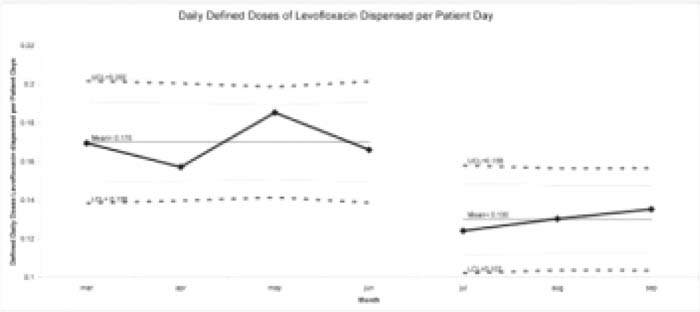
The effects of educational efforts by a physician champion to reduce CDI were studied in a before–after fashion. The baseline period was 4 months, and the postintervention period was 3 months. The interventions consisted of the following: (1) an article written in the physician newsletter; (2) hospital medicine physicians were educated regarding the CDI program, complete with updated guidelines regarding antibiotic choices for diverticulitis and pyelonephritis; and (3) a microbiologist reviewed charts of patients on levofloxacin, the FQ on formulary, on an intermittent basis to gauge appropriateness of use, and notifred the attending physician if appropriate documentation supporting FQ was not found, The total sum of milligrams of levofloxacin dispensed was monitored. The defined daily dose (DDD) of levofloxacin according to the World Health organization is 500 mg. The measure studied for this pilot study is DDDs of levofloxacin dispensed/patient day. Data was tabulated on a monthly basis, and analyzed by using the chi‐square test. SPSS for Windows (version 17.0; SPSS, Inc., Chicago, lL) was used. Statistical process control (SPG) was also used for better monthly graphical representation of the data.
Results:
The DDD of levofloxacin per patient hospital day decreased from 0.17 at baseline to 0.13 after the intervention (P < 0.001).
Conclusions:
A CDI program consisting of education and reminders for hospital medicine physicians reduced levofloxacin use. Further study is needed to determine if the preliminary findings are sustainable, if non‐FQ antibiotic use increased, and if this program definitively reduces CDI.
Author Disclosure:
H. Shabbir, none; J. Stone, none; A. Singh, none; D. Tong, none.