Background: Increasing number of palliative care patients are cared for by hospitalists, but the value of hospitalist on end-of-life (EOL) care is scarcely reported. The study aims to evaluate the effect of hospitalist care on the intensive care utilization and medical expenditure for end-of-life hospitalizations.
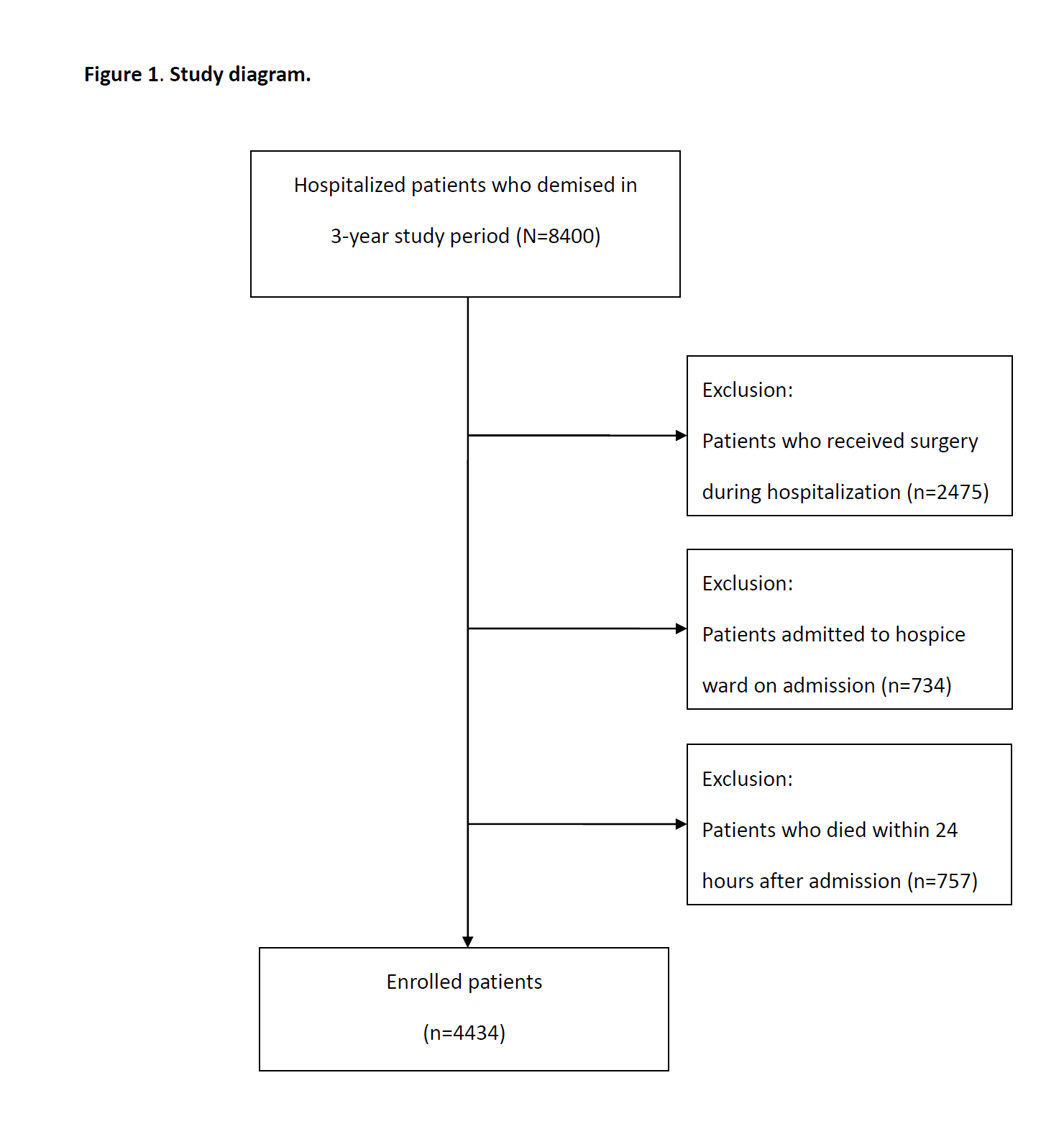
Methods: A three-year retrospective observational study was conducted at a 2400-bed tertiary medical center in Taiwan. All deceased hospitalized adult patients, except for those who received surgery, hospice unit admission and those who stayed less than 24 hours, were enrolled. Patients who received hospitalist care were compared with those who did not in terms of clinical characteristics and survival. Multivariate regression analysis was adapted for the associations between hospitalist care and intensive care unit (ICU) admission, total and average daily medical expenditure with adjustment of covariates, including palliative care consultation meeting.
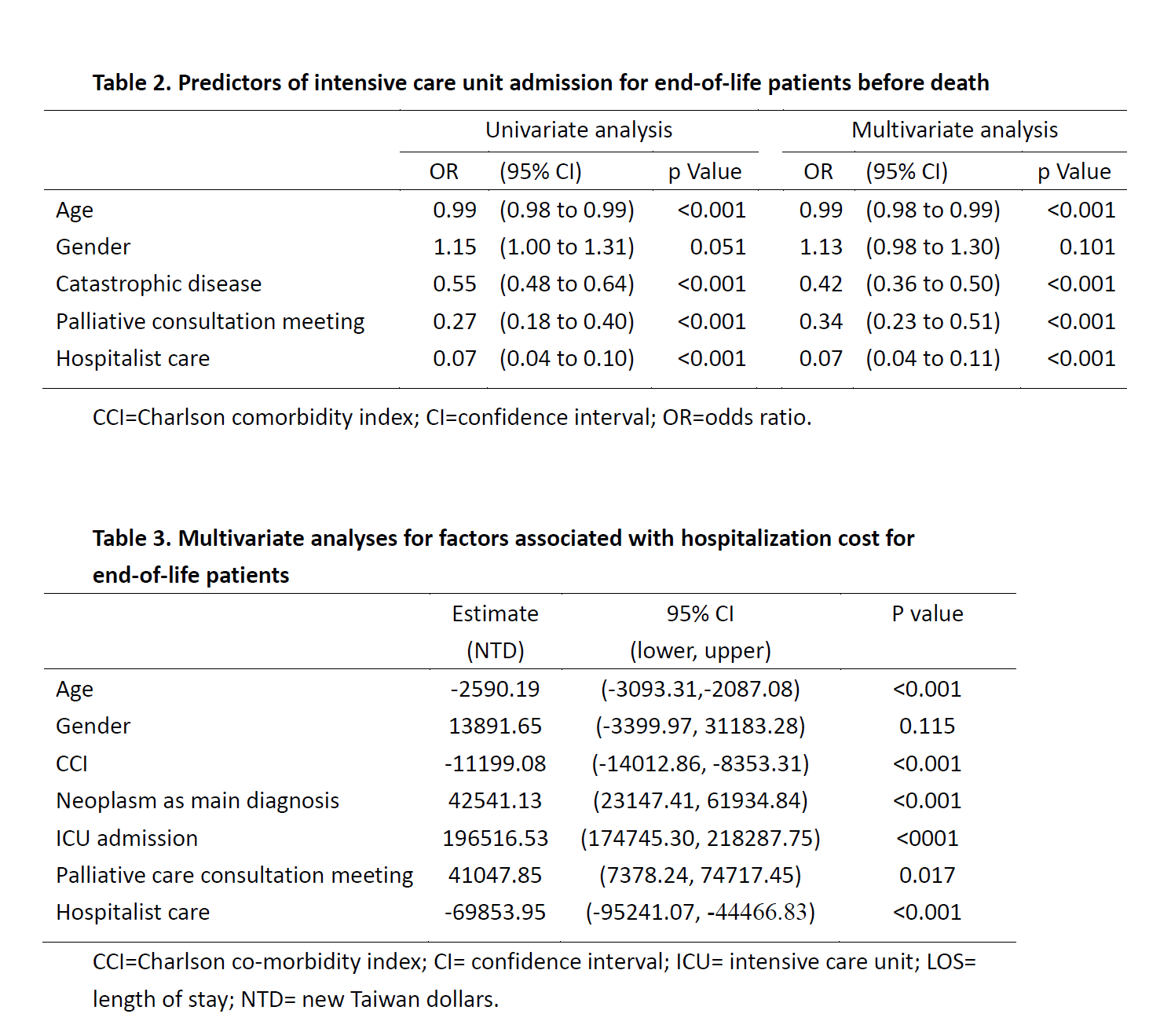
Results: From Jan 2013 Jan to Dec 2015, a total of 4434 patients were enrolled. Of all, 660 patients (14.9%) were cared by hospitalist. Compared to the comparison group, patients who received hospitalization during terminal hospitalization had fewer cancer diagnosis (28.3% vs. 45.3%, p<0.001), and lower Charlson co-morbidity index (3.16 vs. 3.65, p=0.001). However, more palliative care consultation meetings were convened by hospitalists (13.9% vs. 5.9%, p<0.001). After controlling for covariates, the multivariate regression analysis showed that hospitalist care was associated with fewer ICU admission for EOL hospitalizations (OR 0.07, CI 0.04-0.11, p<0.001). Multivariate regression showed that hospitalist care, as compared to non-hospitalist care, was associated with significant lower hospitalization costs (estimate -69853 NTD per admission), while cancer as primary diagnosis (estimate +42541 NTD per admission), ICU admission (estimate +196516 NTD per admission) and palliative consultation meeting (estimate +41047 NTD per admission) were associated with higher hospitalization costs.
Conclusions: Hospitalist care is associated with fewer intensive care before death, and with lower medical expenditure for terminal hospitalized patients.