Background: Emergency room (ER) crowding remains a widespread problem. Hospitalist led transfers for stable patients may be one intervention to improve patient flow and ER overcrowding. There are no prior studies assessing the impact of hospitalist-directed transfers from one ER to an inpatient ward at a different, affiliated hospital on patient flow.
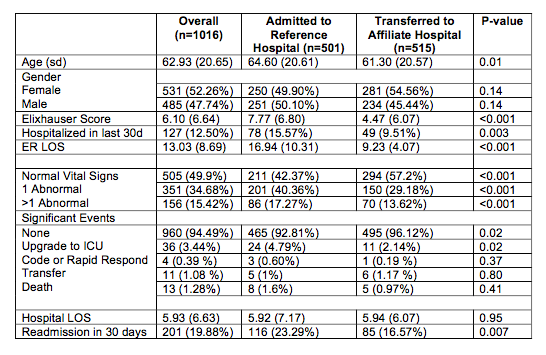
Methods: We performed chart review on 1016 admissions to the hospitalist service. Of these, 501 remained at the reference hospital and 515 represented transfers to the nearby affiliate hospital. Outcomes included ER length of stay (LOS), hospital LOS, adverse events during hospitalization, and 30-day readmission rates.
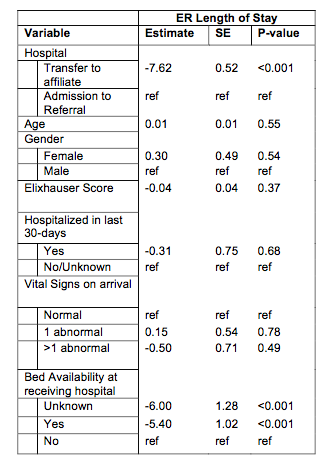
Results: In the univariate analysis, patients who remained at the reference hospital had longer ER stays (16.94 v. 9.23 hrs; p<0.001); greater risk of significant events, specifically to upgrade to ICU care (4.8% v. 2.1%; p <0.001); and higher 30-day readmission rates following their index admission (23% v 17%; p = 0.007). In the multivariate analysis, transferred patients had a shorter ER LOS on average by 7.62 hours (p<0.001).
Conclusions: When compared to routine admissions at a reference hospital, hospitalist- coordinated transfers to inpatient wards at an affiliated hospital are a safe practice that lead to shorter ER LOS and were associated with fewer adverse events. These results are likely dependent on bed availability at the receiving hospital and evaluation by a hospitalist on the patient’s safety for transfer.