Background: Experts identify empathic responses to patient expressions of negative emotion – such as anxiety, sadness, and anger – as a key component of patient-centered communication, yet evidence on the impact of empathy on patient-reported outcomes in the hospital is limited.
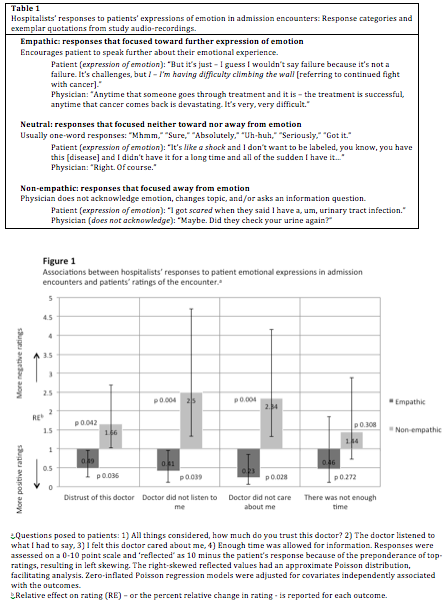
Methods: Our study objective was to assess the association between hospitalists’ expressions of empathy and patients’ anxiety and ratings of the encounter. We audio-recorded 76 patients’ admission encounters with 27 hospitalist physicians at 2 academic hospitals and surveyed patients before and after the encounter. Audio-recordings were coded using previously published methods to categorize how hospitalists responded when patients expressed negative emotion during the encounter; response categories were “empathic”, “neutral”, or “non-empathic” (Table 1). Our primary outcomes were 1) the difference between a patient’s pre- and post-encounter anxiety assessed via the 60 point State Anxiety Scale; 2) patient ratings of the hospitalist and encounter using 7 validated items assessed on a 0-10 scale; and 3) encounter length. We used multivariable linear and Poisson regression models – with robust standard errors to account for clustering by hospitalist – to estimate the associations between each of our outcomes and the frequency of empathic, neutral and non-empathic hospitalist responses in each encounter, adjusting for patient illness severity and pre-encounter anxiety.
Results: Across the 76 admission encounters, there were 190 instances in which the patient expressed a negative emotion (range 0-14, median 1 expression per encounter). Hospitalists responded empathically 32% of the time, neutrally in 43% of cases, and non-empathically in 25%. Each empathic hospitalist response was independently associated with a 1.65 point decrease on the State Anxiety Scale (95% CI 0.48 – 2.82). More frequent empathic responses were associated with more positive ratings of the hospitalist and encounter, while more frequent non-empathic responses were associated with more negative ratings (Figure 1). The number of empathic responses was not associated with encounter length (+1%, 95% CI -8%-10%).
Conclusions: Empathic responses to patients’ expressions of negative emotion were associated with decreases in patient anxiety and higher patient ratings of the hospitalist and encounter, but not longer encounter length. Given empathic communication could have a significant impact on patient experience in the hospital, reinforcement of healthcare providers’ use of empathy has the potential to improve patient satisfaction without sacrificing efficiency.