Background: The majority of medical students indicate that the health policy and health systems education they receive is insufficient, even though they will face barriers to practicing care at the systems level. In addition, there is little uniformity or evaluation of pedagogical approaches to health policy in undergraduate medical education, especially in connecting health policy topics to real-world clinical medicine (1). Case-based learning and small group learning have been shown to be effective for medical students’ learning about pathophysiology and clinical medicine. However, these approaches have not been evaluated for health systems education, possibly due to the perceived lack of expertise of clinical faculty to facilitate discussion about health policy topics. Clinically active hospitalists, even without formal expertise in health policy, may play a role in providing this integration.
Purpose: To pilot the use of hospitalist faculty to facilitate case-based discussions with pre-clinical medical students that illustrate health policy topics and health systems barriers to high quality healthcare.
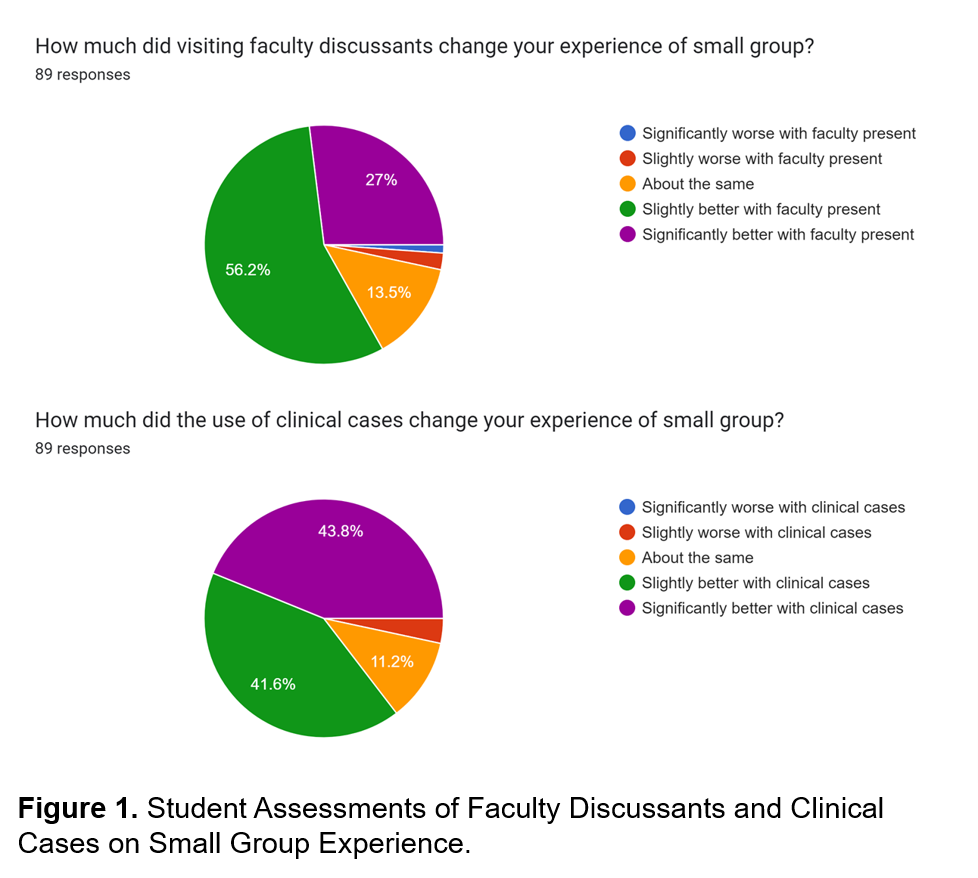
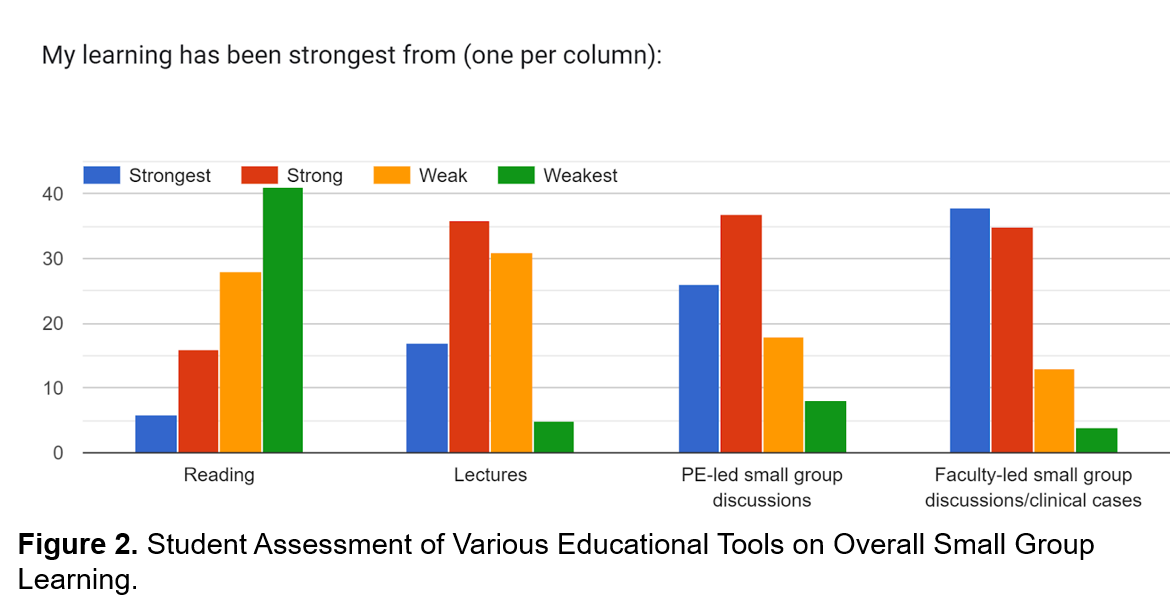
Description: First-year medical students were required to take an introductory course on health policy and the US healthcare system. Topics included the history of public and private health insurance, health economics, provider reimbursement, quality and value, drug prices, and other topics. In addition to didactic lectures, students were divided into small groups facilitated by 4th-year students who served as Peer Educators (PEs). Small groups featured discussions and interactive activities to promote active learning of health policy topics. In 2023, we invited faculty discussants to two out of four sessions to facilitate case-based discussions around high-value care, provider reimbursement, and quality of care. Cases were realistic examples involving barriers to care commonly faced by hospitalists and other providers. Using an optional small group feedback survey administered after all four small group sessions, we compared students’ learning experiences with case-based learning to readings and didactic lectures, and we compared their experiences of hospitalist-facilitated sessions and PE-facilitated sessions. Of 91 first-year medical students, 89 responded to the feedback survey. For sessions on high-value care and physician payment, respectively, 84% and 78% of students agreed or strongly agreed that hospitalist discussants were valuable to their learning. Overall, 83.2% of survey respondents indicated that their small group experience was slightly or significantly better with hospitalists present (Figure 1). Additionally, 85% of respondents indicated that their small group experience was slightly or significantly better when clinical cases were utilized (Figure 1). When assessed on overall learning, 82% of students indicated that their learning was strong or strongest from faculty-led small group discussions and clinical cases compared to only 25% from readings and 60% from didactic lectures (Figure 2).
Conclusions: Hospitalist-facilitated case discussions were rated higher than discussions at which faculty were not present, and faculty-led discussions were rated the highest among several modalities of teaching. This pilot suggests a strong role for hospitalists in health policy for medical students even without formal expertise in these fields.