Background:
Hospital care accounts for more than 30% of health care expenditures in the United States. In an effort to reduce inappropriate admissions, we implemented hospital medicine attending screening of non–intensive care unit (ICU) medicine admissions.
Methods:
We conducted a before and after study at our urban, academic safety‐net hospital. From January to June 2008, all patients admitted to the medicine wards or to the chest pain observation unit were screened by a hospital medicine attending physician, who, in collaboration with referring providers, could change the initially recommended disposition. Patients who were admitted to inpatient medicine and discharged or transferred to the ICU within 24 hours or admitted to medicine after having been discharged within 7 days from the Emergency Department (ED) from January to June 2008 were identified and compared with a historical control from the same months 1 year prior. Two physicians reviewed each chart for appropriateness of disposition. If there was a disagreement, a third reviewer determined appropriateness. Bayesian statistics were used to determine the diagnostic accuracy of emergency medicine providers, and chi‐squared testing was used to compare accuracy pre‐ and postintervention.
Results:
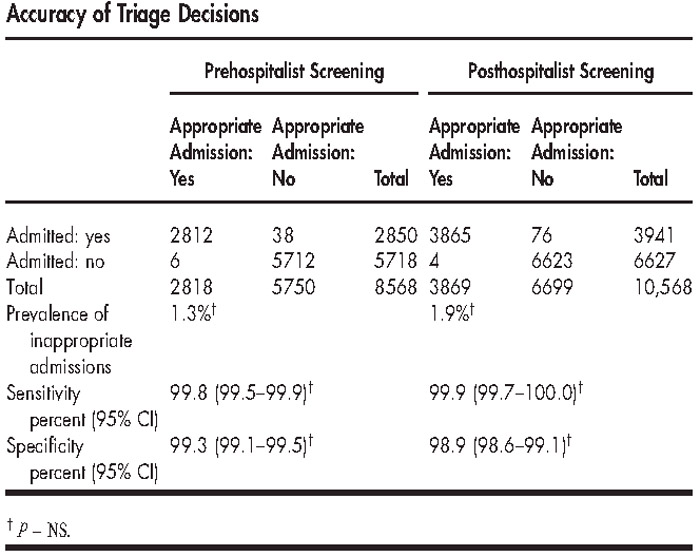
Neither the overall admission rate nor the inappropriate admission rate changed from pre‐ to postintervention (Table). The positive predictive values and negative predictive values of the ED decision to admit were >98% and 99%, respectively, and did not change postintervention. In the postintervention period, 82.5% of triage changes (n = 141) were classified as escalations in care setting. The most common diagnoses were chest pain (n = 78, 46%), pneumonia (n = 11, 6.4%), alcohol withdrawal (n = 8, 4.7%), and sepsis (n = 8, 4.7%). Of triage changes, 17.5% (n = 30) were classified as deescalations of care setting. The most common diagnoses for these patients were chest pain (n = 18, 60%) and deep vein thrombosis (n = 3, 10%).
Conclusions:
Our study suggests that the screening of admissions from the ED by hospital medicine attending physicians is not an efficient allocation of resources. At our institution, inappropriate admissions are relatively rare events. Attempts to further reduce inappropriate admissions may increase inappropriate discharges.
Disclosures:
R. Allyn ‐ none; J. Long ‐ none; L. Shockley ‐ none; B. Cleary ‐ none; A. Keniston ‐none; E. S. Chu ‐ none