Background: Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Health authorities across the country have grappled with how to ensure equitable access for patients. In Victoria, British Columbia, a small group of pioneering community physicians were responding to all community and hospital MAiD requests. The lack of a coordinated system, coupled with an increasing volume of requests, resulted in unintentional barriers to inpatients.
Purpose: A subgroup of the Victoria hospitalists wanted to provide MAiD services to inpatients to supplement the work of the community physicians. They felt that a successful service would provide seamless access, be patient focused, collaborative, and respectful of conscientiously objecting physicians and staff.
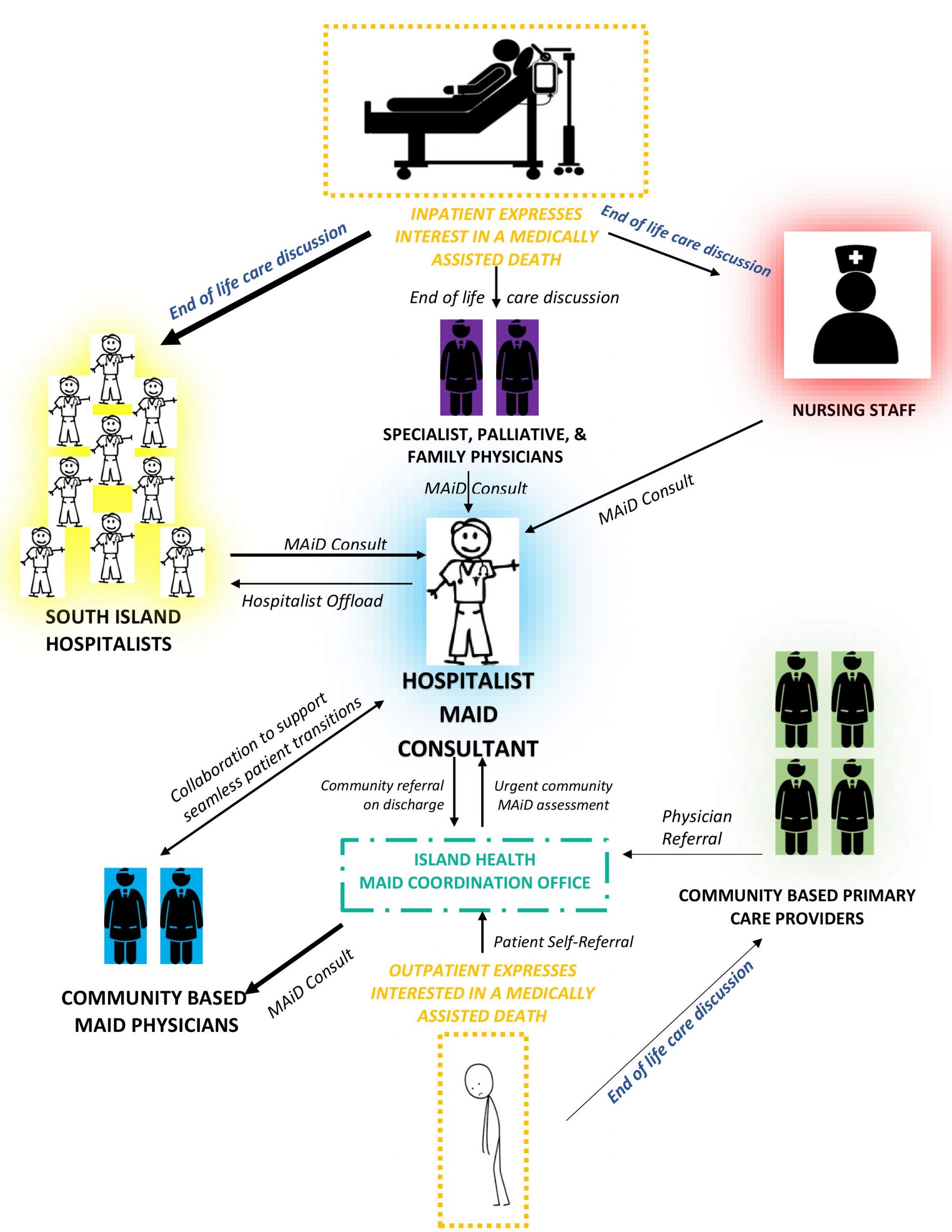
Description: The MAiD legislation requires that eligible patients have a grievous and irremediable medical condition, be capable of informed consent, and have a reasonably foreseeable death. After completion of a formal witnessed written request, patients must be assessed and found eligible by two independent physicians, one of whom is the provider of medical assisted death. Two hospitalists undertook Phase I of the Hospitalist MAiD service pilot project. With financial support from the health authority, these hospitalists began assessments and provisions in addition to regular scheduled work. The intention was to generate data and identify challenges with inpatient provision of MAiD by a hospitalist group. It quickly became clear that the volume of requests could not be sustainably managed as an add-on to a full hospitalist work day. Additionally, several other factors, most notably the need for dedicated time and the need to respect boundaries of conscientiously objecting physicians, led to the development of a formal Hospitalist MAiD Consult Service as Phase II of the trial. Through a series of meetings with the MAiD steering group and input from a variety of stakeholders, the unique Hospitalist MAiD Consult service was conceived. The Hospitalist MAiD consultant is a certified hospitalist physician that attends to all MAiD related work in the three Greater Victoria hospitals. Referrals are received directly from physicians or nurses. In collaboration with the multidisciplinary care team, the consultant provides education, access, and completes MAiD assessments and provisions. In addition to MAiD work, the consultant works alongside hospitalist colleagues, offloading generalist hospitalist work for hospitalists performing MAiD assessments. Knowledge of patient resources, collegial relationships with nursing and allied health staff, and expertise in end of life care make hospitalists well suited to this role. In addition, the consultant liaises with the community physicians to ensure seamless transitions between inpatient and outpatient care, including urgent outpatient assessments.
Conclusions: Medical Assistance in Dying is legal in Canada. Through perseverance and respectful collaboration, this group has created a robust, innovative and sustainable service. With the support of administration and community providers, the Victoria Hospitalist MAiD Consult Service provides streamlined and predictable access to MAiD for inpatients. The feedback from patients, families, specialists, hospitalist colleagues, and administration has been resoundingly positive. And ultimately, the hospitalized patients whose access to assisted death was challenged by their circumstances, now have a reliable opportunity to die on their own terms.