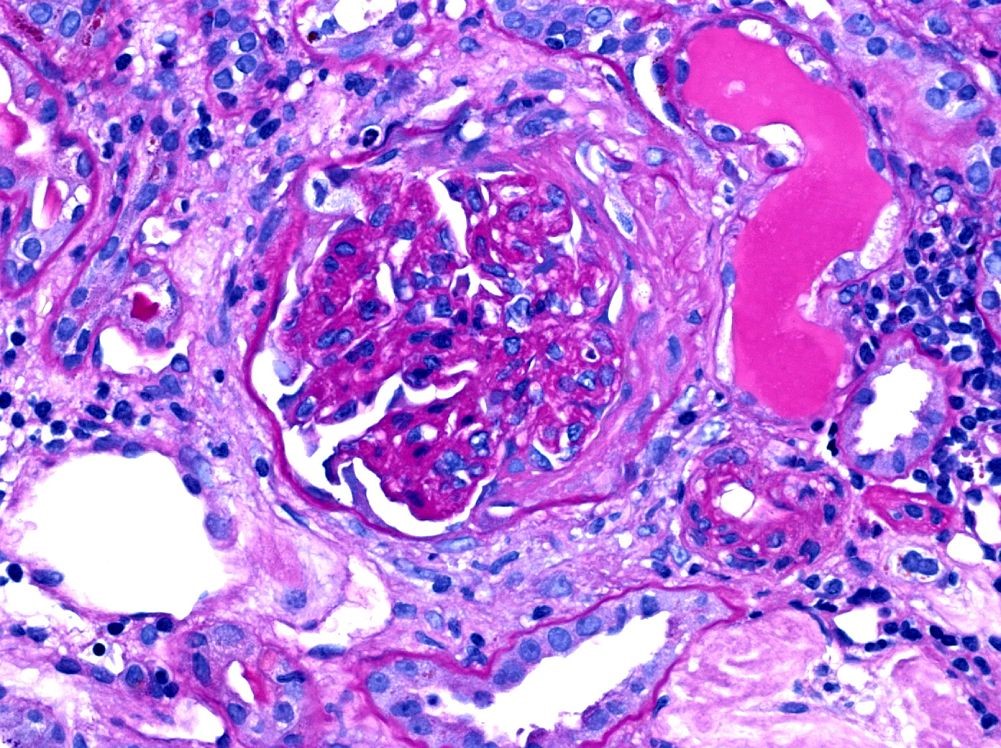
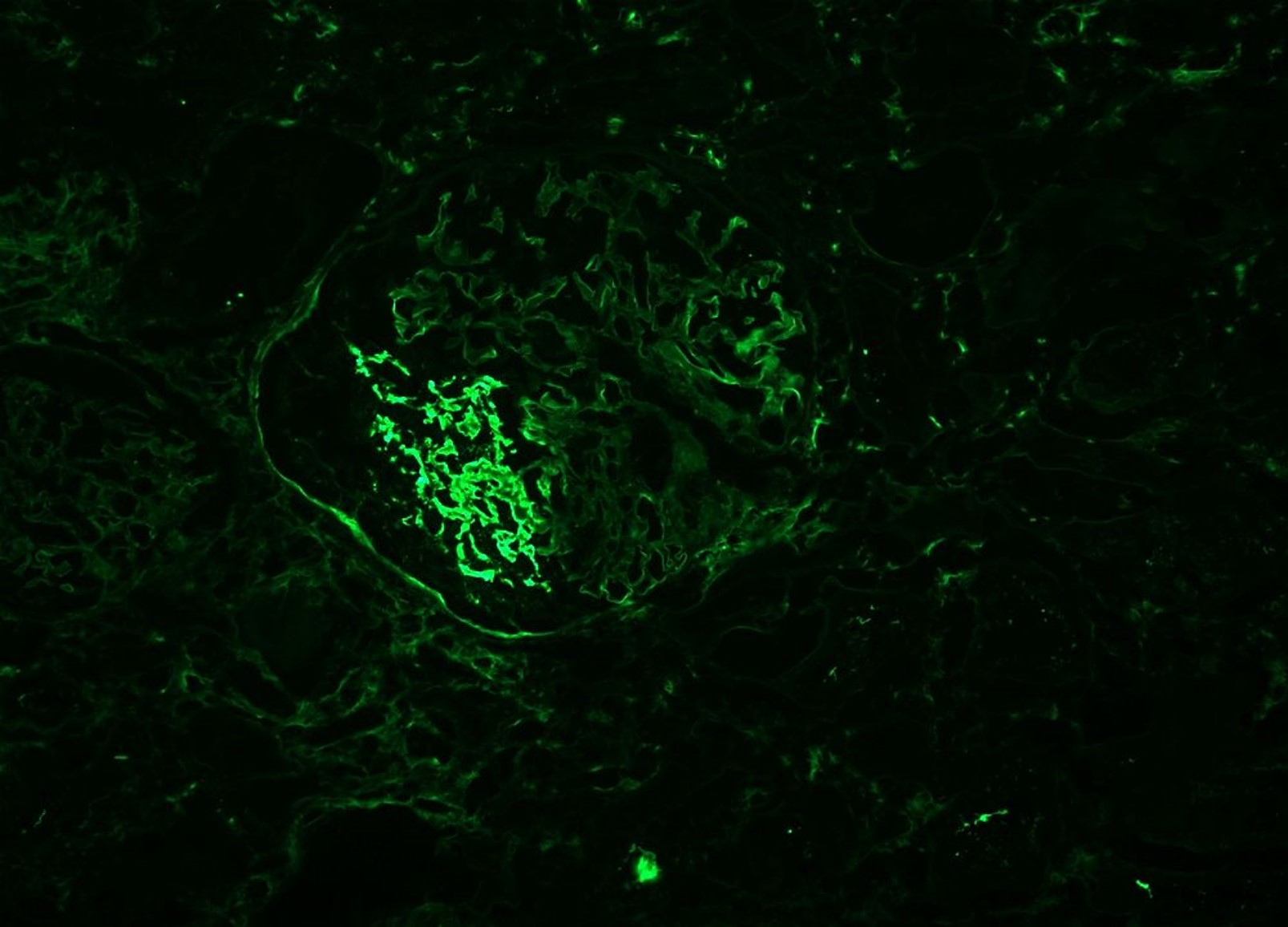
Case Presentation: We present a 79-year-old female treated with hydralazine for essential hypertension who initially presented to her primary care office with non-specific complaints of malaise, chills and unintentional weight loss. Routine laboratory evaluation was performed indicating a substantial rise from the patient’s baseline creatinine of 0.86mg/dL to 2.15mg/dL. Follow-up labs indicated continued worsening of renal function, and the patient was admitted for further evaluation. Preliminary laboratory work-up revealed an ESR >100mm/hr, p-ANCA 1:320 and MPO >100. Given these findings and systemic symptoms, systemic vasculitis, particularly an ANCA associated vasculitis was high on the differential. A kidney biopsy was performed that showed evidence of focal necrotizing and crescent glomerulonephritis pauci-immune type, acute tubular injury and mild diabetic glomerulonephropathy class IIa. Hydralazine was immediately discontinued given the concern for drug- induced ANCA associated vasculitis, microscopic polyangiitis specifically based on the ANCA testing. After initial treatment with high dose steroid therapy, the patient was induced with 1g rituximab for initial and eventually transitioned to scheduled rituximab infusions. The patient’s renal function continued to improve with her last creatinine reported at 1.83mg/dL. The patient never required dialysis.
Discussion: We presented a unique case of hydralazine-induced vasculitis. The exact pathogenesis is still unknown although several leading hypotheses include the binding of hydralazine to myeloperoxidase (MPO) leading to neutrophil apoptosis and antibody production, reversal of epigenetic silencing of MPO leading to an increased expression of neutrophil auto-antigens, or breakdown in tolerance in slow vs. fast acetylators of hydralazine. Though the exact mechanism remains unclear, the buildup of leukocytes within the vessel walls compromises the lumen leading to eventual tissue ischemia and necrosis. Vasculitis itself is defined by size, type and location of the vessels it affects. Furthermore, it can be defined as a primary or secondary vasculitis. Specifically, ANCA, or anti-neutrophil cytoplasmic antibody, associated vasculitis is the result of a necrotizing process, not the deposition of immune complexes. Of ANCA associated vasculitis patients, 10-20% will have renal disease at the time of presentation with 77-85% eventually developing it. A kidney biopsy is essential in the confirmation of the diagnosis as well as predicting disease severity and progression. Given the vagueness of presenting symptoms, it is important to proceed with kidney biopsy to confirm diagnosis, when applicable. Confirmation of diagnosis can lead to prompt discontinuation of the offending agent, as well as prompt initiation of therapy in hope to defer long term renal disease and possible dialytic needs. Recent studies have also indicated better prognosis in patients treated with newer immunosuppressive agents, including rituximab.
Conclusions: Hydralazine, commonly associated with drug-induced lupus, is less commonly associated with drug-induced ANCA associated vasculitis. The occurrence of systemic vasculitis in association with hydralazine use, though a rare complication, may have devastating consequences if not detected early. With this case, we hope to bring awareness to hydralazine’s association with ANCA associated vasculitis.