Background: Rapid Response Teams (RRTs), also known as medical emergency or patient response teams, are widely implemented in hospitals to improve patient outcomes. Existing literature demonstrates that RRTs reduce in-hospital mortality, cardiac arrest, and unplanned ICU admissions. However, less is known about the outcomes of patients transferred to the ICU following an RRT activation. At our institution, a critical care support nurse (CCRN) may be deployed at the conclusion of an RRT event to provide one-on-one, ICU-level care for patients who require ICU but for whom there is no immediately available ICU bed, or the CCRN may continue to temporize patients within their current level of care to avoid an ICU transfer. Evidence supporting and optimizing this practice is limited.
Methods: In this single-center, retrospective quantitative study conducted at a large, 1,100-bed academic hospital, we evaluated the outcomes of patients who underwent an unplanned ICU transfer following an RRT activation over a 23-month period (November 2021 – October 2023). We performed manual chart reviews for all patients who transferred to the ICU and were either de-escalated to a lower level of care or died within 24 hours of ICU transfer. Data were collected on the service line, RRT activation reasons, and the type and duration of critical care interventions post-ICU transfer. Additionally, we assessed whether utilization of the CCRN could have prevented the ICU transfer, based on whether critical care interventions in the ICU lasted 6 hours or less.
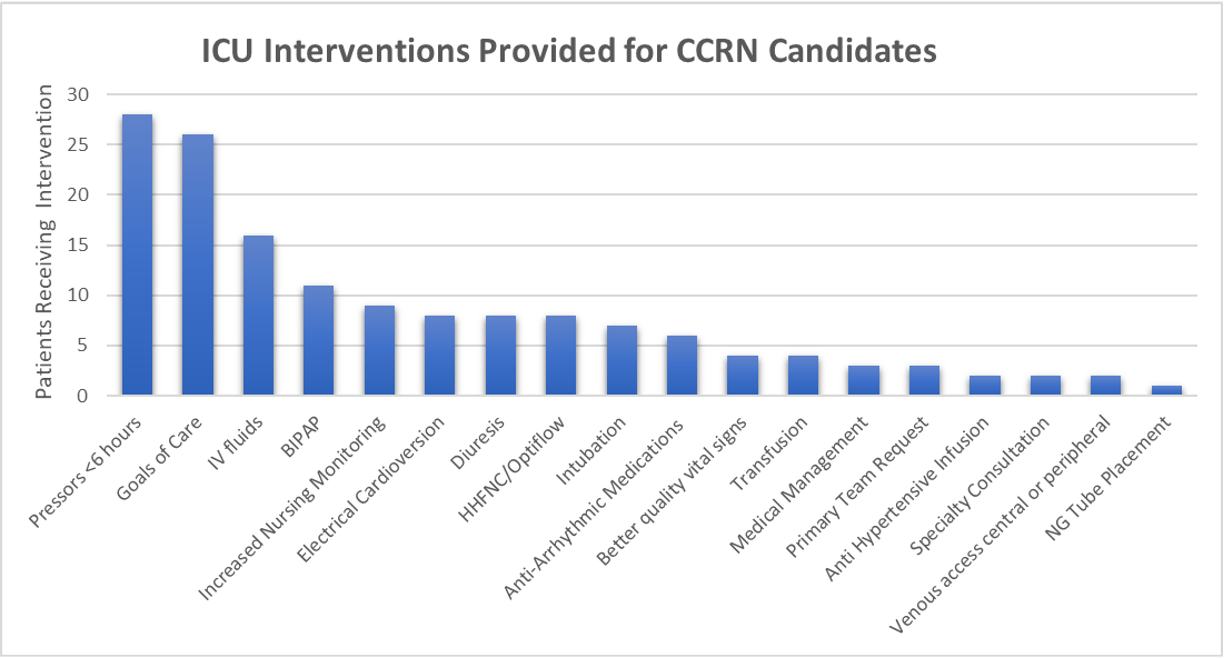
Results: A total of 1,848 RRT activations led to ICU transfers. Of these, 169 (9.1%) patients experienced a de-escalation of care within 24 hours of ICU transfer. Among these, 106 (62.7%) were identified as potential candidates for CCRN intervention, where resuscitation or temporization could have been achieved outside the ICU. Populations particularly suited for CCRN support included patients transitioning to comfort care (26%) and those requiring short-term vasopressor use (28%). Additional subgroups included patients needing cardioversion, noninvasive ventilation, intravenous fluids, or increased nursing care. Our findings suggest that many patients who underwent rapid de-escalation of care after RRT and ICU transfer could have been managed without ICU transfer, highlighting opportunities to optimize CCRN utilization at our institution.
Conclusions: This study found that nearly 10% of patients transferred to an ICU following an RRT event transition back to a lower level of care or die within 24 hours after transfer. Specific patient populations that may benefit from CCRN intervention to avoid ICU transfers include patients transitioning to comfort care, and patients requiring short-term vasopressor support. These findings suggest that refining RRT protocols to better utilize CCRNs could improve care efficiency and patient outcomes, potentially reducing unnecessary ICU admissions.