Background: Stigmatizing language in clinical notes can negatively impact physician attitudes, propagate bias, affect prescribing behaviors, and exacerbate healthcare disparities, yet remains prevalent even in the Open Notes era. Prior analyses of stigmatizing terms in clinical notes are limited by the lack of context in which terms are used and multiple meanings of certain words such as “resistance”, which can refer to a stigmatized behavior, antibiotic treatment, or joint examination. We sought to (1) identify terms almost always used in a stigmatizing context and (2) determine if racial and ethnic disparities exist in the use of these context-specific stigmatizing terms.
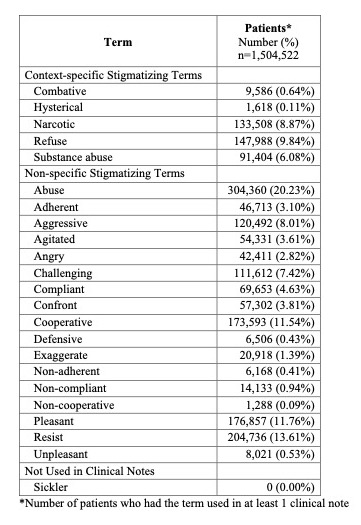
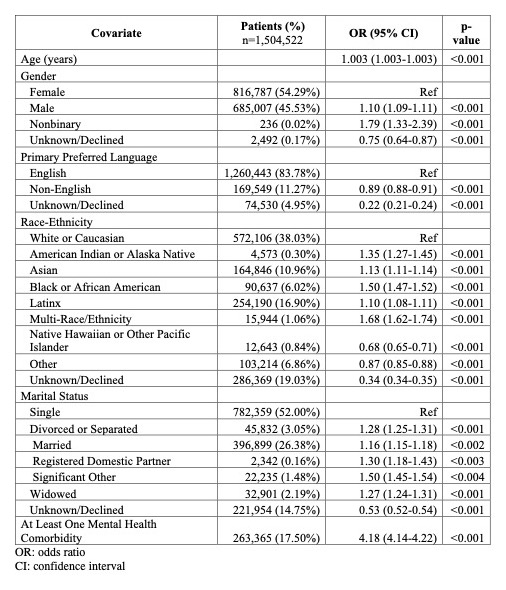
Methods: We assessed the prevalence of 23 stigmatizing terms previously identified in the literature in clinical notes written between January 1, 2015 and June 30, 2022 using our tertiary academic medical center’s Deidentified Clinical Data Warehouse. We manually reviewed 50 sample notes with each term to determine whether the term was used exclusively in reference to a stigmatized patient behavior or characteristic (context-specific stigmatizing terms) or used in other clinical contexts as well. We performed multivariable logistic regression to analyze the association between patient-level demographics, mental health comorbidities, and use of a context-specific stigmatizing term in at least one clinical note for a given patient.
Results: We analyzed over 80 million notes from 1,504,522 unique patients. Of the 23 searched stigmatizing terms, 5 were used to describe patients in consistently stigmatizing contexts: “combative” (9,586 patients), “hysterical” (1,618), “narcotic” (133,508), “refuse” (147,988), and “substance abuse” (91,404, Table 1). One term (“sickler”) was not found in any notes, and 17 terms were used in multiple contexts, which were not specific to a stigmatized patient behavior or characteristic. Use of the 5 context-specific stigmatizing terms, in aggregate, was more frequently associated with male gender (OR: 1.10, CI: 1.09-1.11) and non-binary genders (OR: 1.79, CI: 1.33-2.39) compared to female gender (Table 2). Patients identified as American Indian or Alaska Native (OR: 1.35, CI: 1.27-1.45), Asian (OR: 1.13, CI: 1.11-1.14), Black (OR: 1.50, CI: 1.47-1.52), Latinx (OR: 1.10, CI: 1.08-1.11), and Multi-race/ethnicity (OR: 1.68, 1.62-1.74) were associated with greater stigmatizing language compared to those identified as White. The strongest association with greater use of stigmatizing language was presence of a mental health comorbidity (OR: 4.18, CI: 4.14-4.22).
Conclusions: To our knowledge, this is the first study analyzing stigmatizing language in clinical notes in a context-specific manner. Only a subset of stigmatizing terms described in the literature were consistently used in a stigmatizing context. These terms were found to be differentially utilized by gender, race, ethnicity, and the presence of a mental health comorbidity. This list of context-specific stigmatizing terms will inform initiatives to decrease use of stigmatizing language in the EHR. Next steps include a broader analysis of context-specific use of other stigmatizing terms, revision of standard note templates to remove these stigmatizing terms, and development and implementation of a custom EHR dictionary to assist clinicians by flagging stigmatizing terms and suggesting alternatives at the time of note-writing.