Background: Electronic Health Records (EHR) systems are broadly used to support the delivery of patient care and to facilitate communication and coordination among providers. The use of EHR has been demonstrated to improve health care quality and efficiency. However, the impact of how providers utilize EHRs and communicate information in care delivery remains unclear. Specifically, how do EHR systems shape the patterns of communication between providers? Does information exchange in EHR indicate emergence of care teams? What types of outcomes are likely to be affected by communications taking place in EHR systems?
Purpose: The purpose of this study was to 1) test the feasibility of using EHR access data to identify care teams and 2) characterize communication patterns in care teams using social network analysis.
Description: This study was conducted at a large academic medical center, and was approved by its Institutional Review Board. A random sample of 100 surgical colorectal cancer patients receiving treatment between 2013 and 2014 were selected. We extracted detailed access logs information from the EHR system to create a chronological dataset of provider access to the sample patients’ EHR records. The data include encrypted patient identity, encrypted user (i.e., provider) identity, clinical role of the user, date and time of access, and action performed on the record.
For each patient, we created a communication tie between two providers who accessed the patient’s EHR records consecutively, and used such communication ties to construct a patient-centered communication network. We used Gephi, a social network visualization tool, to visualize the communication networks. We calculated betweenness centrality, which is a structural indicator of how central a provider was in a network based on his/her position on communication pathways between other providers, for selected patients’ communication networks; and identified care teams that consisted of providers with the highest centrality.
For the 100 patients, there were 5075 unique providers (physicians, nurses, technicians etc.) involved in their care, and 267,826 communication ties.
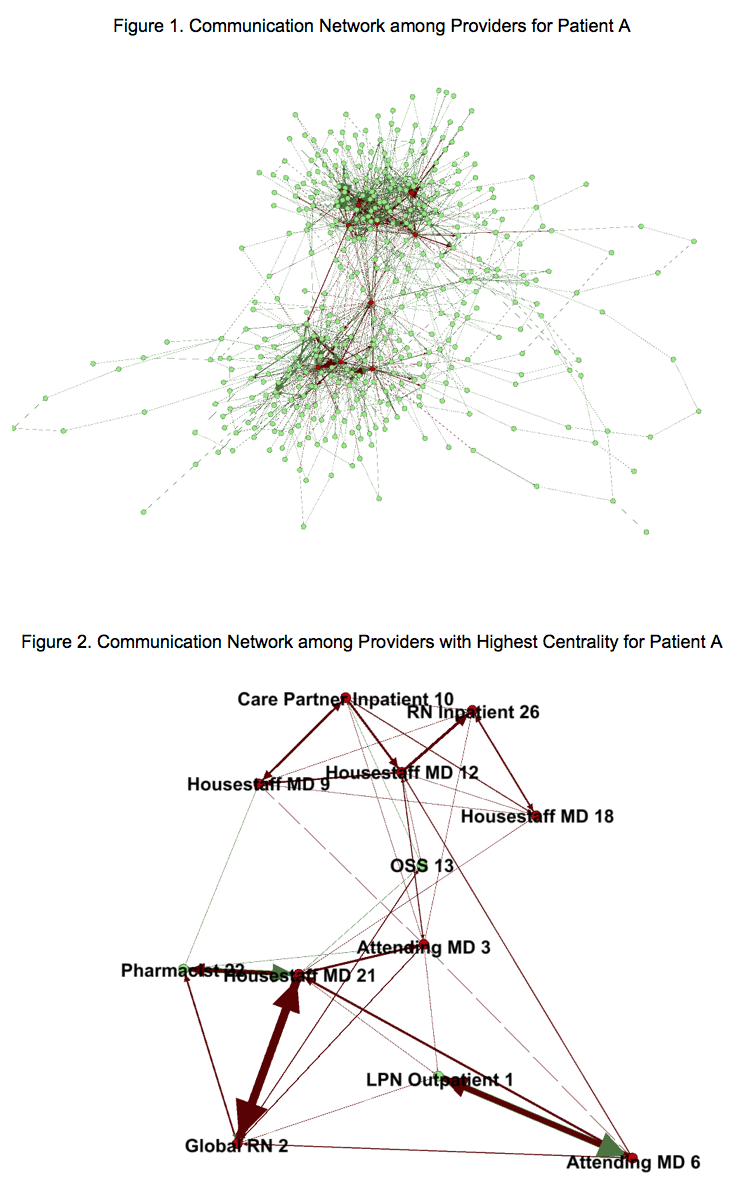
Figure 1 shows the communication network of all providers who accessed patient A’s EHR records. This network consists of 433 providers and 1,826 communications ties. The average path length (i.e., the average minimum number of ties needed to connect any two providers) is 4.2. Figure 2 shows communication ties between 12 distinguishable providers who have the highest centrality in the communication network, which we identify as the care team for patient A.
Examining the network structure in Figure 2, we find that: 1) Attending MD 3 is the most central provider in this network; 2) most frequent communications (indicated by the width of the tie) does not involve the most central provider; and 3) the team can be structurally divided into two components – the outpatient component (lower half of the network) and the inpatient component (upper half of the network) that are primarily connected through Attending MD 3.
Conclusions: The EHR access data provide rich information on patterns of communication between providers. Using social network analysis, it is feasible to identify and examine structural characteristics of care teams that emerge from the large communication networks. Future study is needed to examine the implications of team characteristics on care coordination and patient outcomes.