Background: Equity is an essential domain of healthcare quality [1] but is rarely addressed within quality measurement programs. Quality initiatives, without explicit equity focus, may exacerbate underlying disparities.[2]To address this historic lack of focus on equity, the Centers for Medicare & Medicaid (CMS) now provides confidential reports to hospitals on two disparity metrics for Medicare & Medicaid dual-eligible patients [3]: (1) the Across-Hospital readmission disparity metric compares readmission rates for dual-eligible patients across hospitals & (2) the Within-Hospital readmission disparity metric reports the difference in readmission rates between dual & non-dual eligible patients within a hospital. These methods can also be applied to assess disparities in race or other factors. Understanding how disparities relate to overall quality will help inform how quality programs incorporate disparity metrics. Therefore, we used the CMS disparity methods to (1) identify hospitals that provide equitable 30-day readmission rates by patient race (Black vs. white) or insurance (dual vs. non-dual eligible) and (2) examine the relationship between equitable readmission compared to value of care (quality & cost) and other indicators of hospital quality.
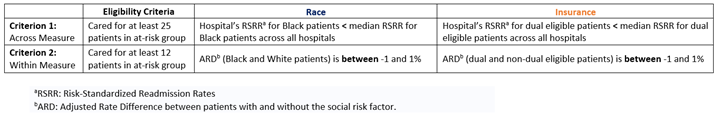
Methods: This is a retrospective cohort study using 7/2018-6/2019 Medicare Standard Analytic Files of all hospitals eligible for the CMS Hospital Wide Readmission (HWR) measure. We classified hospitals as having equitable readmission if (1) the hospital’s risk-standardized readmission rate for the at-risk group (Black or dual-eligible) was better than the median performance for that group across all hospitals (Across-Hospital); & (2) the absolute difference in readmission rates between the at-risk & not at-risk group was < 1% (Within-Hospital). Eligibility criteria are detailed in the Table. We used logistic regression to examine the bivariate association between equitable readmission classification against value, quality, and cost. High overall quality was defined as receipt of 4 or 5 stars in the CMS Hospital Quality Star Rating Program.[4] Low cost was defined as being in the lowest cost quintile using the CMS MSPB measure.[5] High value, consistent with prior work,[6] was defined as having both high quality & low cost. Additional quality domains for Safety, Readmission, Mortality, Patient Experience, and Timely & Effective Care were also examined.
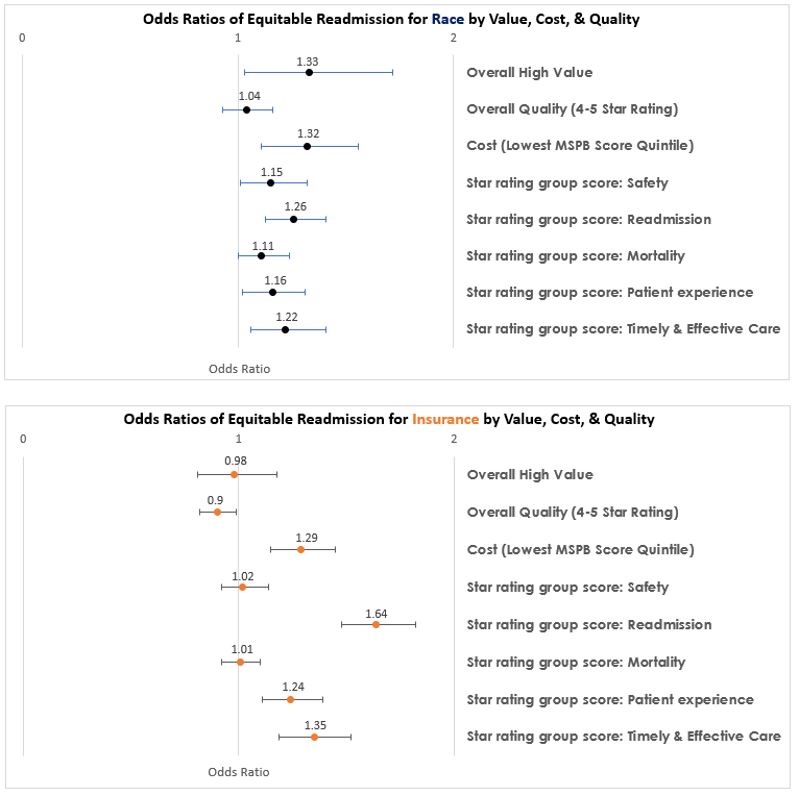
Results: Of 4767 hospitals in the CMS HWR measure, 1967 (41%) were eligible for the equitable readmission metric by race and 3414 (72%) were eligible for the equitable readmission metric by insurance. 464 (23.6.%) of hospitals were classified as having equitable readmission rates by race, & 592 (17.3%) by insurance. Equitable readmission by race was associated with higher value & lower costs, but not overall quality (Figure). Equitable readmission by insurance was not associated with value or overall quality but was associated with lower costs. When examining specific measures of quality, equitable readmission by race or insurance was associated with lower overall readmissions, better patient experience and efficiency, but not mortality.
Conclusions: Hospitals with equitable readmission rates by race have better performance on overall quality & value, but this pattern is not as consistent for hospitals with equitable readmission rates by insurance. Categorizing hospitals by value & quality alone does not sufficiently capture hospitals’ performance on outcome equity.