Background:
Improving discharge planning is a high priority in hospital medicine. There are numerous studies on discharge checklists, follow‐up phone calls, standardization of communication between inpatient and outpatient physicians, and links between improved follow‐up and better outcomes. We explored the role of nonphysician extenders by adding a patient service representative (PSR) to our nonfeaching hospitalist service in February 2008. The PSR is a nonclinical, clerically trained staff member focused on patient‐centered discharge planning, working personally with patients to make follow‐up appointments and communicating with their physicians. We hypothesized that the use of this novel, cost‐effective resource would improve quality of care.
Methods:
One thousand and eighty‐five patients having a diagnosis of CHF, COPD, or DM and discharged from July 2007 to September 2008 were included in the retrospective analysis. Administrative data were combined with data from 2 other hospital databases. Primary outcome variables were readmission rates to hospital within 30 days of discharge and length of stay. Secondary outcomes were time of discharge, percentage of discharges before noon, and patient satisfaction on discharge‐related metrics. In a subset of 442 patients, emergency department (ED) visits within 30 days and number of scheduled follow‐up appointments were examined. Data were also analyzed to determine if increasing comorbidity (total number of conditions out of CHF, COPD, DM), age, disposition plan, or insurance status had anv significant impact on outcomes.
Results:
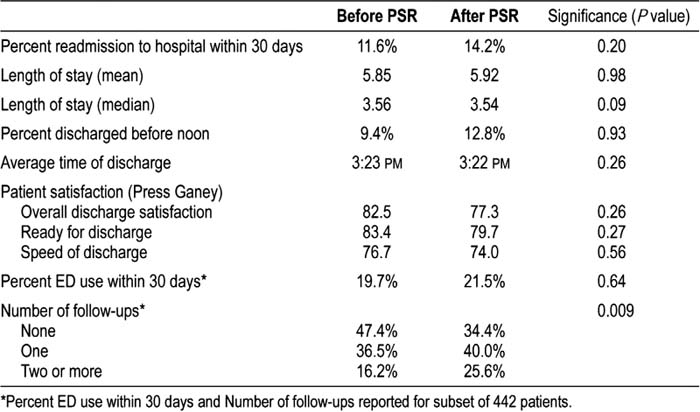
Primary outcome variables of 30‐day readmissions and length of stay did not improve, nor did secondary outcomes (time of discharge, number of discharges before noon), although there was a nonstatistically significant improvement in prenoon discharges. In a subset of 442 patients, number of return ED visits in 30 days was not different, but there was a significantly higher number of follow‐up appointments made after the PSR started (Table 1). In subgroup analysis, it appeared that both increasing age and increasing index of comorbidity increased length of stay and 30‐day hospital and ED readmission but that the PSR did not improve these in the postintervention period. Disposition and insurance status had no consistent impact on outcomes. Patient satisfaction scores did not improve.
Conclusions:
A patient service representative significantly increased the number of follow‐up appointments scheduled in discharged high‐risk medical patients bui did not have a measurable impact on other outcomes. Further study is required to determine whether this improvement in follow‐up improved quality of patient care in other ways.
Author Disclosure:
E. King, University of Pennsylvania School of Medicine, employment; D. Cottrell, Hospital of the University of Pennsylvania, employment; S. Kasi, University of Pennsylvania School of Medicine, student; M. Cary, University of Pennsylvania School of Medicine, employment; L. Shawhughes, University of Pennsylvania School of Medicine, employment.