Background: Troponin is a big molecule, with its fragments not readily cleared by impaired renal function or during dialysis [1]. Oftentimes diagnosing myocardial injury/infarction (MI) is challenging in patients with ESRD due to atypical clinical features coupled with indeterminate ECG changes [2], and elevation of troponin levels with lower PPV [3]. In this study, we aim to look at the relationship between elevated troponin in ESRD patients and its diagnostic value in myocardial infarction as well as the composite outcomes among the patients studied including mortality and 30 day readmission rate.
Methods: In this retrospective single center study, we utilized electronic chart review from April 2020 till November 2021. We included patients over 18 years old admitted with ESRD and elevated Troponin T, excluding trauma patients and out of hospital cardiac arrest. During this period a total of 277 patients were included. We collected data on patients´ age, ethnicity, gender, comorbidities, smoking and drug status, diagnosis, length of hospital stay, access and type of dialysis. Baseline, admission, peak and percentage of increased troponin were analysed. Using The Fourth Universal Definition of Myocardial Infarction we divided ESRD patients between MI and elevated troponin levels based on their admission and peak troponin levels. The increase of troponin above the 99th percentile on admission was considered elevated. An elevation of troponin above 20% from admission was considered as MI. Using a multivariate model that adjusts for confounding factors, we evaluated the association between mortality up to 1 year and 30 day readmission rate between these 2 groups.
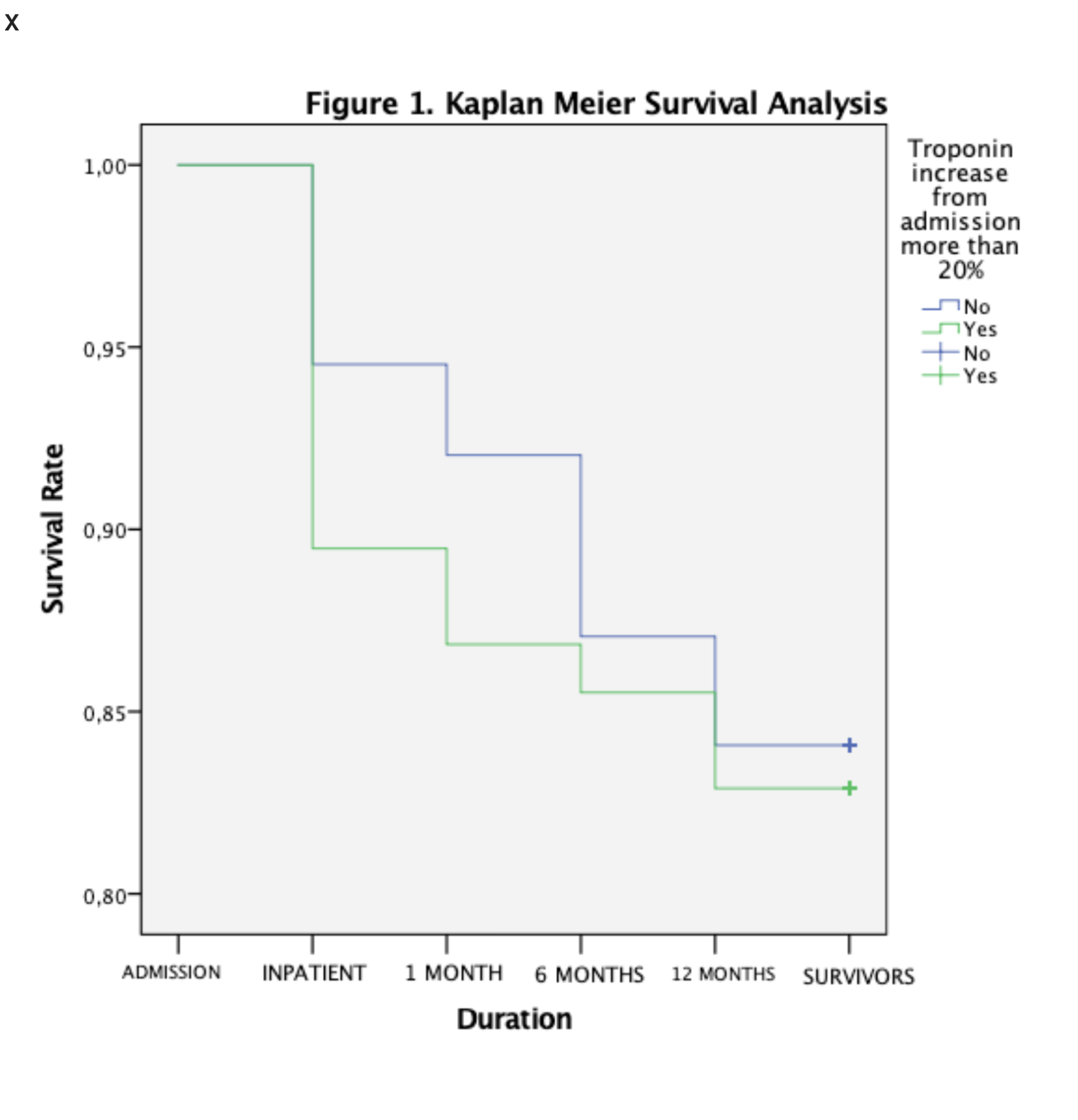
Results: Of the 277 patients included , 76 met the criteria for MI, the rest were defined as elevated troponin. The majority of patients in both groups used AVF as their method for dialysis and the most common admitting diagnosis in patients with ESRD and MI was infection. 13 patients with MI expired compared to 32 of 201 patients with elevated troponin (p=0.413). The Kaplan-Meier curve showed that patients with ESRD and MI have a marginally significant association regarding inpatient mortality (15.2% vs 5.7%; p=0.046). There was no significant difference between both groups regarding total readmission rate within 30 days (23.1% vs 17.3%; p=0.114), all other cause (19.5% vs 10.1%; p=0.091) and CV readmission ( 3.6% vs 7.2%; p=0.296).
Conclusions: In our study, significant (>20% elevation inpatient from baseline) troponin elevation in patients with ESRD could be associated with early phase mortality (within 1 month), however there is no clinical and statistical significance in all cause mortality at 6 months and 1 year or readmission rate regardless of the cause between these two groups. Taking the fact that there is no difference between the baseline characteristics, a stable elevation of troponin is as severe as the subgroup being diagnosed with MI in the long run possibly from an ongoing myocardial injury from various causes. Our limitation lies in the fact that there is no certain method of diagnosing mortality from CV cause per se as there is no difference in the mortality rate between the two cohorts analyzed and there is no postmortem to confirm the exact cause.