Background:
Hyponatremia (HN) is the leading electrolyte abnormality among hospitalized patients. In the absence of symptoms, HN is often overlooked as a condition that warrants aggressive intervention. However, a careful history often reveals symptoms associated with HN. Although HN is common, little is known regarding the influence of HN on patient outcomes and health care resource utilization. The present study was designed to identify the impact of HN on length of stay (LOS), inpatient mortality, and cost variables in a hospitalized patient population.
Methods:
This retro spective analysis used the Premier's Perspective® database to select hospitalizations with HN (serum sodium ≤ 135 mmol/L as defined by primary or secondary ICD‐9 276.1) for the January 2007 to June 2009 time frame. Patients transferred to/from another acute care facility and who left against medical advice, and labor/delivery patients were excluded from this analysis. HN patients (n = 564,723) were matched to a non‐HN control by age, sex, provider region, and 3M APR‐DRG assignment. Matching was refined using propensity scores on other patient and hospital characteristics and patient comorbidities. Matched patients were assigned to HN and non‐HN groups for comparisons of total hospital cost, intensive care unit (ICU) cost, length of stay, ICU length of stay, rate of ICU admission, and inpatient mortality rate.
Results:
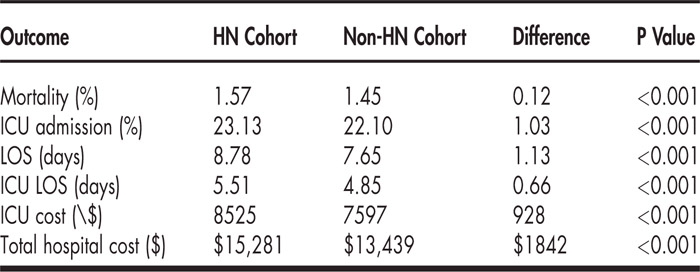
Hospital demographics were similarly distributed across both cohorts. Approximately 57% of the patients came from hospitals located in the South Atlantic, Middle Atlantic, and Pacific regions. Sixty percent of hospitals were nonteaching. Patient demographics included: 57% female, mean age of approximately 68 years, and 41% hypervolemic with comorbidities of heart failure and/or cirrhosis in approximately 48% of both cohorts. A hospitalist attended to 43% of all patients. HN contributed to an increased LOS, increased total and ICU hospitalization costs, increased percentage of patients requiring an ICU admission, increased ICU LOS, and increased inpatient mortality.
Conclusions:
In a hospitalized population, HN was associated with a statistically significant negative impact on inpatient mortality, ICU admission, and total/ICU LOS. HN was also associated with significantly increased total hospital and ICU costs.
Disclosures:
A. Amin ‐ Otsuka, research funding, speakers bureau; S. Deitelzweig ‐ Otsuka, research funding, speakers bureau; J. Lin ‐ Otsuka, consultant; K. Belk ‐ Otsuka, consultant; D. Baumer ‐ Otsuka, consultant