Background: The Accreditation Council for Graduate Medical Education (ACGME) sets strict guidelines governing work hours for internal medicine trainees, not to exceed 80 hours per week. Though many programs grapple with achieving adherence, few published studies report successful changes to meet these limits. Previous efforts at our institution to reduce patient census on the teaching service had only been partially effective at reducing work hours. Following repeated citations by the ACGME for 80-hour violations, we restructured our inpatient medicine teaching service to better comply with work hours limits. Major changes to the 8-team teaching service structure included: transition to a day/night system from 28-hour call, reduction in admitting hours on long call day (5pm instead of 8pm end), set sign-out times based on the day in the call cycle, change to a 28-day rotation (from 1-month), and addition of a fifth day off per rotation for each trainee. We aimed to assess the impact of the new structure on trainee work hours.
Methods: Work hours were measured by mandatory self-reported hours through an online platform (Medhub) and aggregated for all trainees (interns and residents) on the inpatient medicine teaching service. Census data was obtained via Clarity. T-tests were used to compare data before and after the restructure.
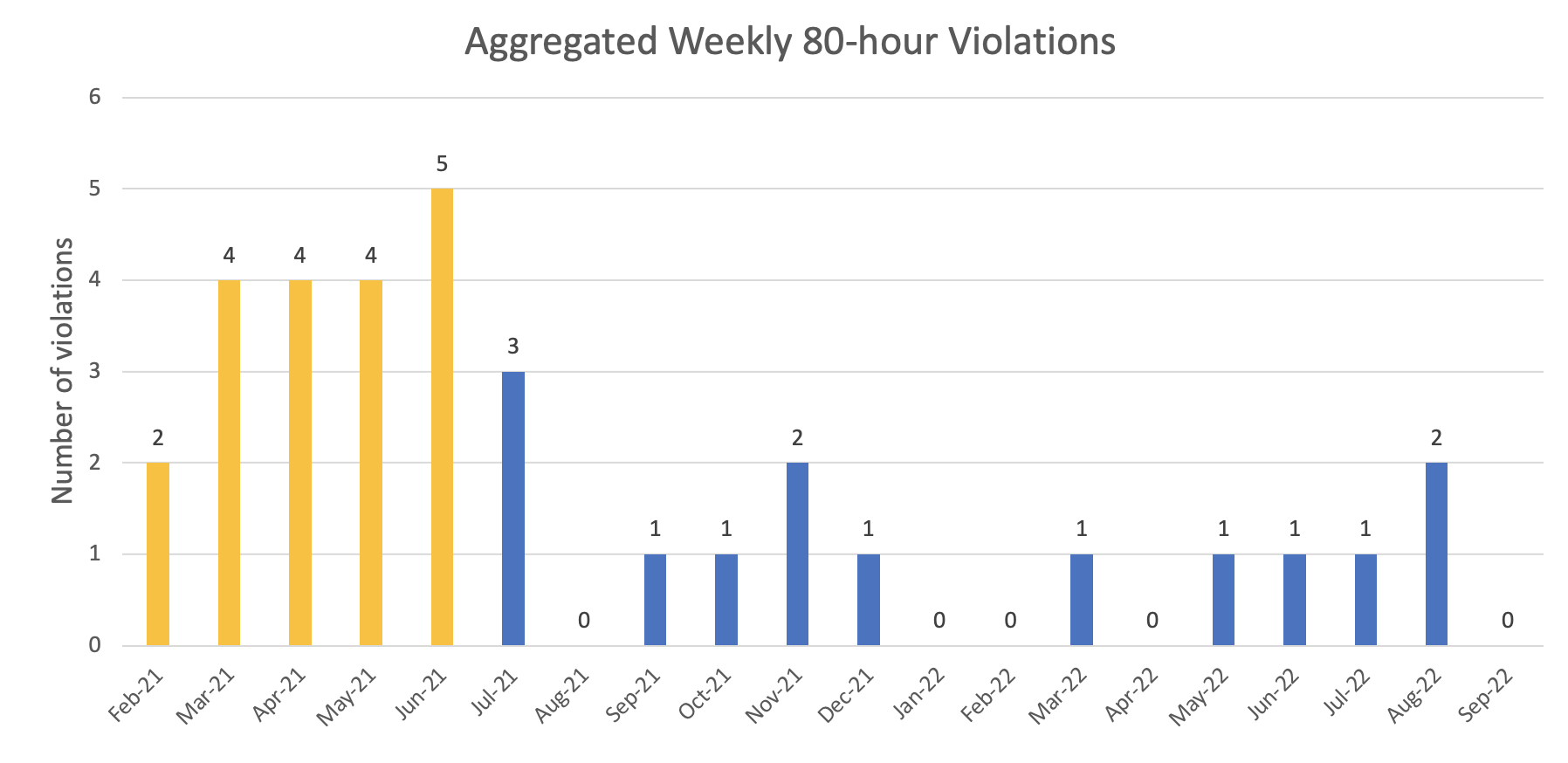
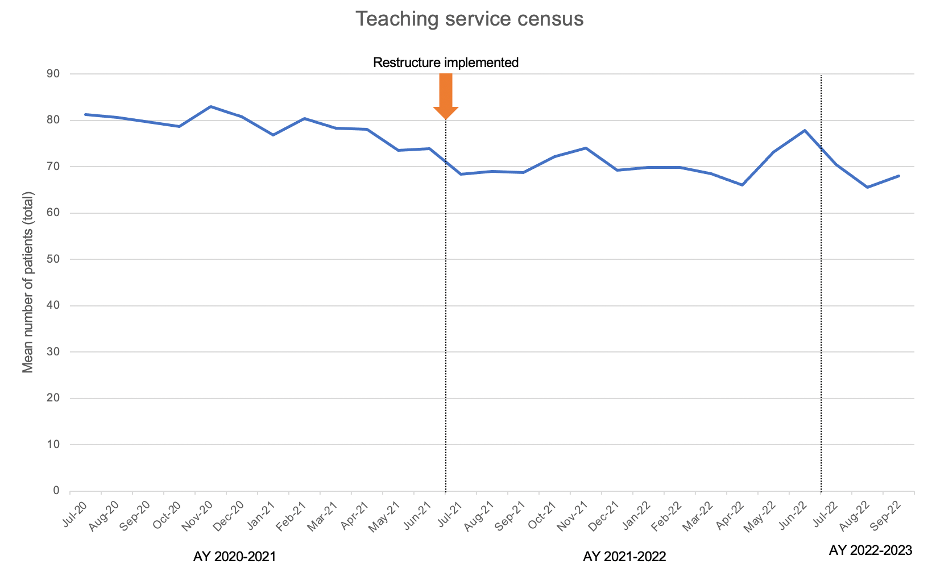
Results: After implementation of the new wards structure, work hour violations by intern and resident trainees on the teaching service fell dramatically: from July 2021-September 2022, there was an average of 0.93 weekly violations for exceeding 80 work hours in a week compared to 3.8 for February-June 2021 (p< 0.001) (Figure 1). Following the implementation of the restructure in July 2021, there were no violations for working more than 80 hours per week when averaged over 4 weeks, compared to an average of 1.8 violations/month from June 2020-June 2021 (p=0.007). Work hour violations for working more than 28 hours decreased from 7 violations/month to 0.2 violations/month following the restructure (p< 0.001). Violations for fewer than 8 hours between shifts were 2.6 violations/month prior to the restructure and 3.4 violations/month after the restructure (p=0.51). Violations for fewer than 1 day off in 7 days were 0.33 violations/month prior to the restructure to 0.19 violations/month (p=0.55) after the restructure. There was a significant reduction in the mean overall census on the teaching service from 78.8 patients in AY20-21 to 70.6 patients in AY21-22 (p< 0.001).
Conclusions: A major restructure of the inpatient medicine teaching service led to a dramatic reduction in work hour violations, with significant reductions in violations for exceeding 80 work hours per week and exceeding 28 hours in a shift. Although census reduction was not an explicit part of the restructure, the overall census on the teaching service fell by 8 patients (average of 1 patient/team), most likely due to a reduction in overall admitting hours on long call. As the overall medicine patient numbers did not decrease, the care for these patients was shifted to non-teaching teams. Further study is needed to determine the differential impact of individual aspects of the restructure and whether work hour improvements can be sustained at higher patient volumes.