Background: UC Davis Medical Center is a 646-bed tertiary care center and level 1 pediatric and adult trauma center, serving over 33 counties. Most inpatient internal medicine consultations originate from orthopedic and trauma services, with a significant subset of fragility fractures and geriatric patients. We established a co-management service to provide additional assistance for the orthopedic trauma service given their complex, predominantly geriatric population. Prior to the initiation of a co-management service, orthopedic surgery patients could receive a traditional internal medicine consultation.
Methods: The data was collected from an Epic Caboodle data warehouse and utilizes patient claims data. The data includes all cases billed as inpatient that had a billed procedure performed by an orthopedic trauma surgeon from January 2020 to September 2024. The co-management service began in September 2021.
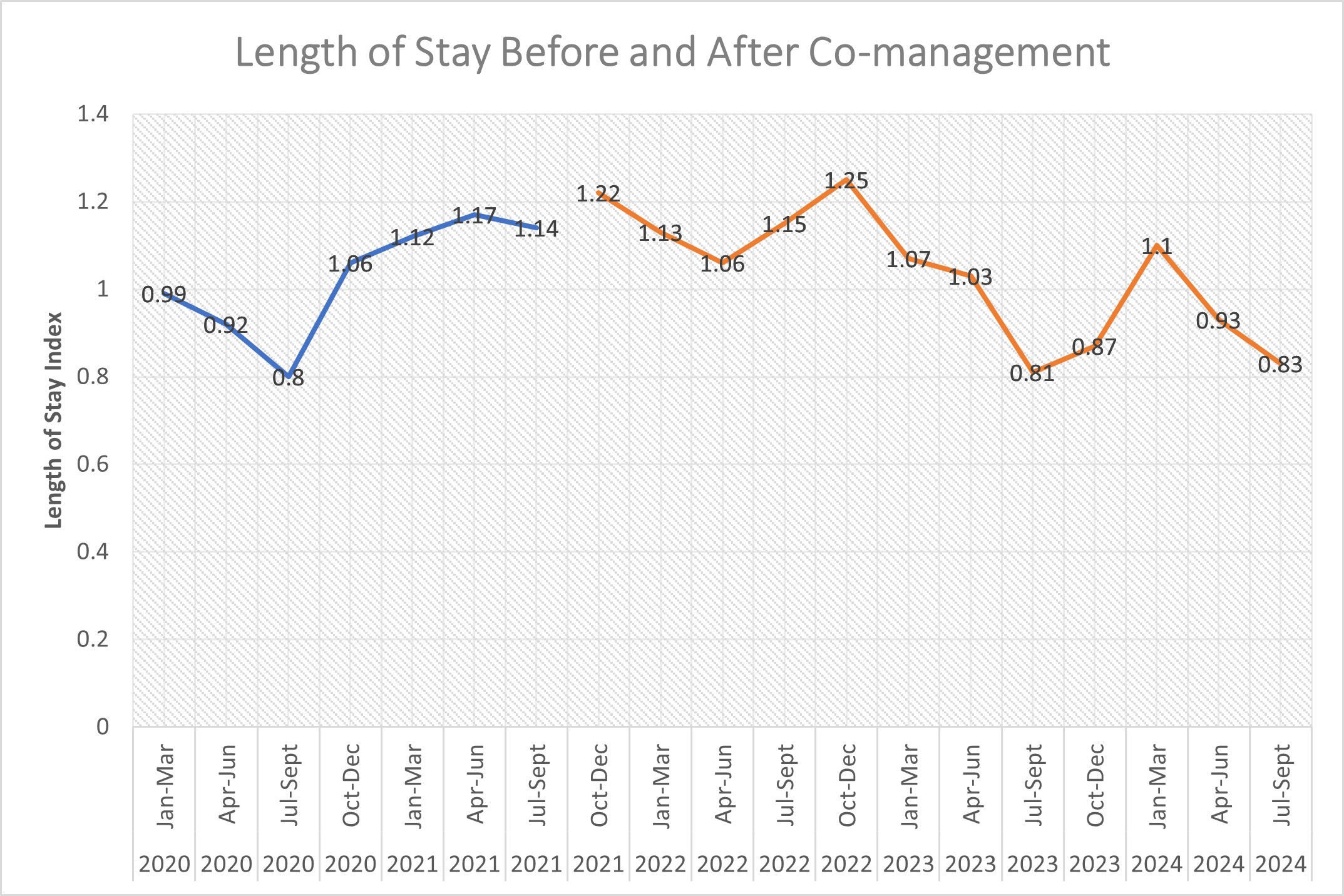
Results: We found that after the co-management service began, patient complexity increased on the orthopedic trauma service as identified by the case mix index. The case mix index (CMI) is a metric used to measure the acuity and severity of illness of a patient population with higher values indicating a higher acuity and sicker patient. Prior to the initiation of a co-management service, the mean CMI was 2.26 which increased to 2.42 (p=0.0047) with co-managed patients having a mean CMI of 2.58 and patients who were not co-managed with a mean CMI of 2.29 (p=< 0.0005). Despite an increasing case complexity, the average length of stay compared to expected length of stay (LOS index) did not significantly change from 1.035 to 0.986 (p=0.57). When comparing co-managed patients with non-co-managed patients, we saw that the average LOS index for co-managed patients was lower at 0.92 compared with 1.06 for non-co-managed patients (p=0.14).
Conclusions: The case complexity managed on the orthopedic trauma service has increased since the initiation of our co-management model. This supports reports from our surgical colleagues that co-management allowed surgeons to feel more comfortable managing a more complex patient population given the increased support from a co-management model when compared with a traditional consultation model. As expected, the patients who were comanaged were significantly more complex than patients who were not comanaged. Despite this increasing case complexity, the length of stay when compared to expected length of stay has remained stable. Interestingly, despite managing more complex patients, the average LOS index for co-managed patients was lower than patients who were not co-managed, although this was not statistically significant. Additionally, the initiation of the orthopedic-hospitalist co-management service had multiple indirect benefits that we did not initially anticipate. The relationship between hospitalists and the orthopedic department improved overall. Increasing face time between the surgical and hospitalist groups allowed for increased partnerships between our departments to increase appropriate inpatient initiation of bisphosphonate therapy, improve early pain control for patients with fragility fractures, and improve the transfer process between services. With the success of our co-management service, there has been a dramatic increase in the desire from other departments as well to collaborate on care for complex surgical patients throughout the hospital.