Background: Accurate clinical documentation is necessary for many aspects of modern health care, including excellent communication, quality metrics reporting, and legal documentation. However, since coding rules and terminology differ from common clinical language, there is a risk that the clinical reality will get lost in translation. This is where clinical documentation improvement (CDI) programs come in. We aimed to assess the impact of our CDI intervention by comparing (CPT) error percentage and Financial Error Rate in a Hospitalist Department before and after implementation of our CDI program.
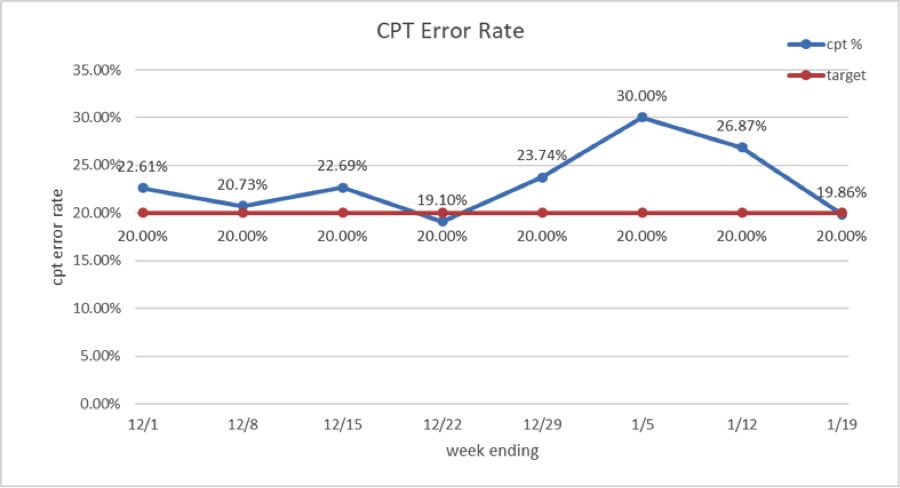
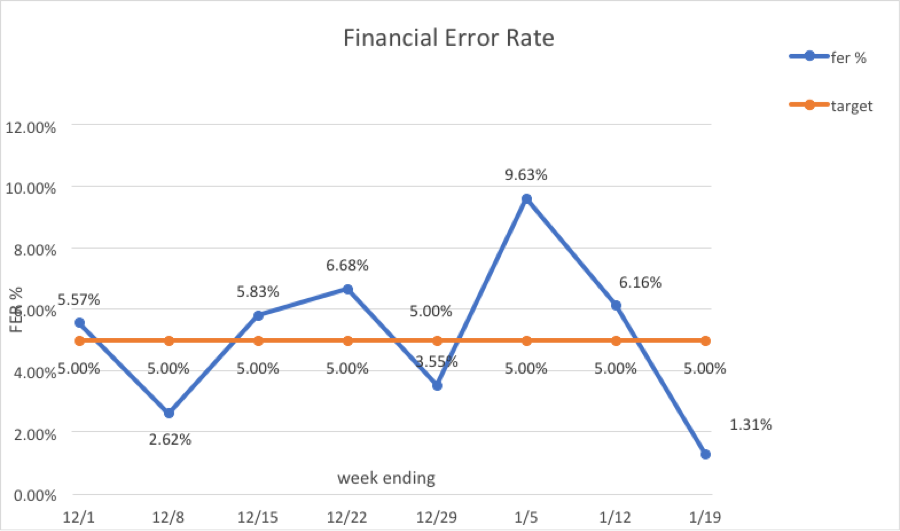
Methods: A CDI intervention was instituted in December 2019 for all members of our hospitalist team. All the charts of hospitalist groups were reviewed by coding analyst. The intervention consisted of emailing weekly write off reports containing individual provider name, date of service, provider CPT code, reviewer CPT code, difference of fee and detailed individual comments for each act of omission. Weekly CPT error percentage and financial error rate was calculated. Educational material was provided to each provider with optional one to one session with lead coding analyst.
Results: CPT error rate dropped from 22.61% to 19.86%Financial error rate dropped from 5.57% to 1.31%
Conclusions: Clinical documentation improvement intervention in form of weekly write off reports in a Hospitalist Department is an effective method to improve CPT error rate and Financial Error rate.