Background: Procedural complications are a common source of adverse events in hospitalized patients(1, 2). In academic centers, bedside procedures have traditionally been performed by trainees, often without experienced proceduralist supervision, or referred to interventional radiology or consultant services, often with an associated delay in procedure performance. Many trainees report discomfort with their skill in performing and supervising procedures(3-5). In order to address these concerns, a number of centers have established medicine procedure services (MPS)(6-10). Our objective was to report our five-year experience after establishing a hospitalist run MPS, including procedural volume, complication rates, and revenue.
Methods: We conducted a retrospective analysis of all patients referred to the MPS for a procedure between 2014-2018. We performed manual chart review for all encounters to identify complications of large volume paracentesis, thoracentesis, central venous catheterization, and lumbar puncture by residents and attending MPS physicians. Charts were reviewed for immediate (within 72 hours of procedure) and delayed complications. We queried hospital medicine billing data for CPT codes for procedures performed by our MPS both before and after implementation of the MPS.
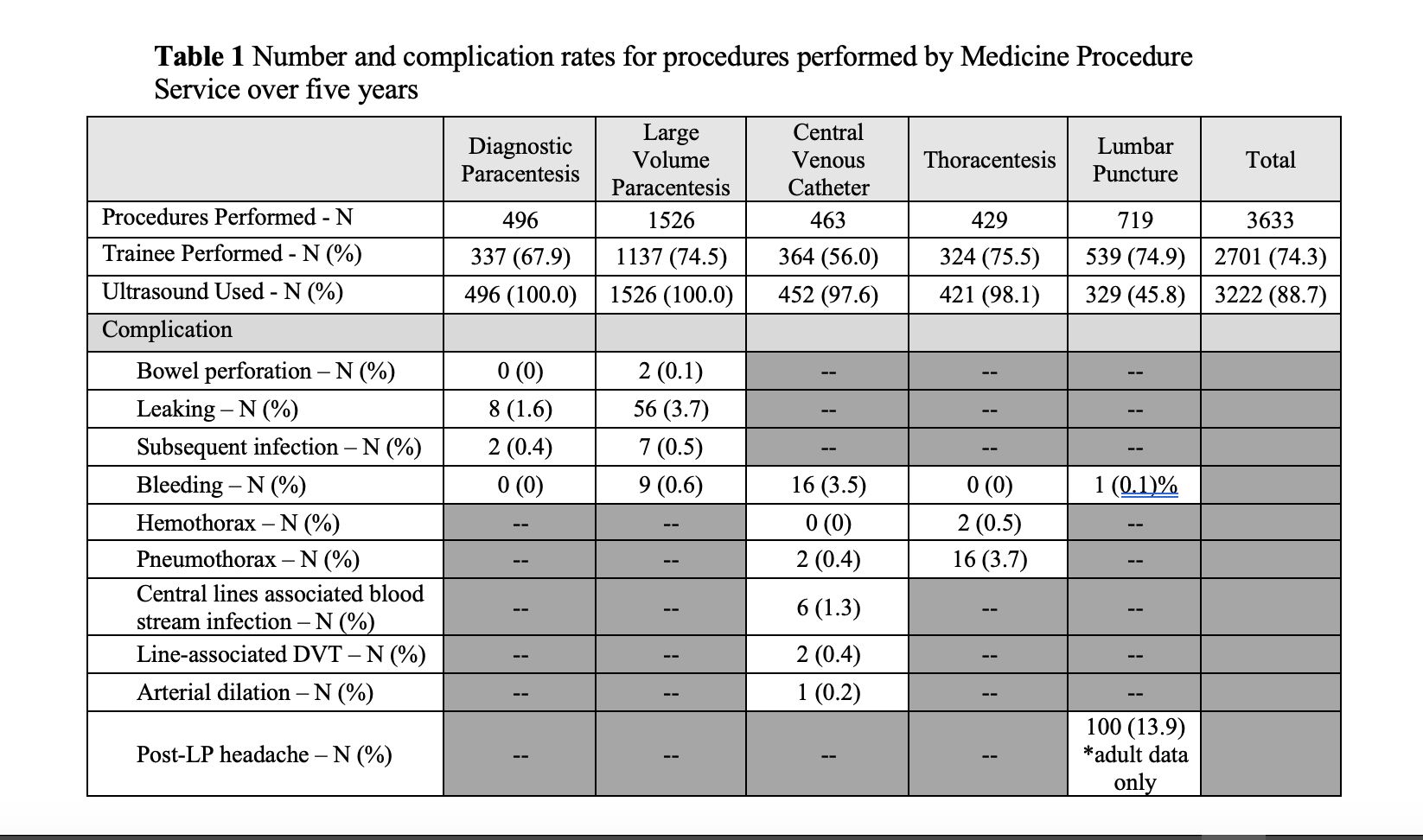
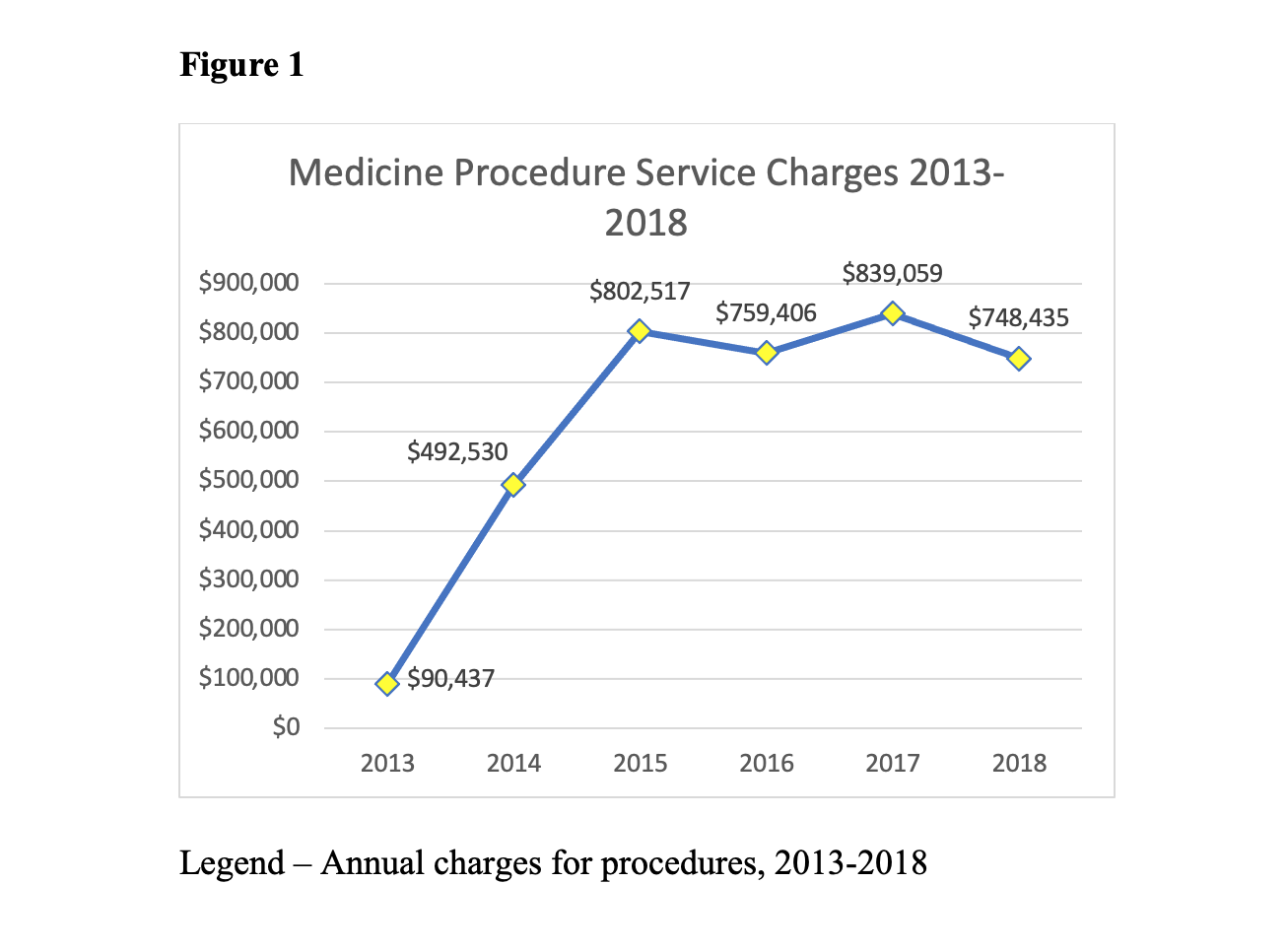
Results: The MPS performed 3,633 procedures with large volume paracentesis being the most common (Table 1). Trainees performed 74.3% of procedures, which were ultrasound-guided 88.7% of the time. Thoracentesis was complicated by pneumothorax in 3.7% of cases, with only 0.5% complicated by bleeding. Bleeding accompanied only 0.1% of lumbar punctures. Post-dural puncture headaches occurred in 13.9%. Leaking was the most common complication for paracenteses (1.6% diagnostic, 3.7% large volume) and bleeding was the most common complication of central venous catheter placement (3.5%). Our complication rates compared favorably to those previously published(10). Prior to initiation of the MPS in 2013, our department’s procedural charges totaled only $90,437. After MPS initiation, charges steadily increased, averaging $787,352 in the last 4 years of the study period (Figure 1).
Conclusions: Implementation of an MPS at our institution resulted in a large volume of procedures, high rate of trainee participation, low rates of complications, and steady increase in procedural revenues over five years. Wider adaptation of this model at academic centers has great potential for furthering trainee education while providing safe procedural patient care.