Background: The patient population at tertiary hospitals is increasingly complex due to advancements in healthcare and more aggressive management of comorbidities. This complexity is particularly evident in the patients on medicine services that have a tracheostomy. Patients with tracheostomies on general medical floors often experience prolonged lengths of stay and multiple inpatient complications, such as mucus plugging and tracheitis(1). The care of patients with tracheostomies presents unique challenges, and many providers report feeling uncomfortable with tracheostomy care and receiving inadequate education on the topic. Research has shown that even senior internal medicine residents often have similar experience and education in tracheostomy care as medical students, highlighting a significant gap in training(2).Given these challenges, a well-coordinated multidisciplinary team (MDT) is now recommended in national guidelines to improve patient outcomes, including reducing length of stay (LOS) and complications(3). Hospitalists are particularly well-positioned to lead these teams due to their comprehensive understanding of complex medical conditions and their ability to coordinate care across various specialties.
Purpose: The goal of this project is to implement a standardized tracheostomy care plan, consistent with evidence-based best practices(3) with the assistance of a MDT, including respiratory therapists (RT) and speech language pathologists (SLP). With this team, we hope to help expedite time to decannulation if applicable, which will in turn decrease tracheostomy complications and patients’ LOS.
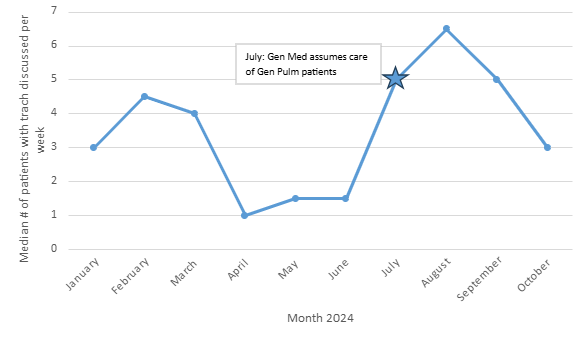
Description: Starting in January 2024, an MDT including a hospitalist, RT, and SLP have met weekly to discuss all General Medicine patients at a single academic university hospital that have a tracheostomy. We discuss barriers to discharge and whether patients are decannulation candidates. If opportunities are identified, the hospitalist directly communicates with the patient’s primary provider to discuss next steps, such as capping trials or more frequent tracheostomy changes. From January through October 2024, we discussed 54 unique patients with a tracheostomy in our MDT. The number of patients discussed weekly rose substantially starting in July as General Medicine assumed care of the primary pulmonology patients at our institution (Figure 1). Of these 54 unique patients discussed thus far, 17 (31%) were able to be decannulated during that admission. This is in comparison to fiscal year 2023 (FY23) where only 11 of 78 unique patients (14%) patients were decannulated (Figure 2).
Conclusions: Early data from the tracheostomy MDT show that there has been a trend toward higher proportion of decannulations, which can help remove barriers to discharging these complex patients. There is still significant opportunity for improvement to decrease time to decannulation for eligible patients and thus decrease their LOS. Future steps will include tracking time between steps toward decannulation, including speaking valve and capping trials. With the continued use of this MDT and increasing tracheostomy education for learners and hospitalists, we wish to improve the care of this medically challenging population at our institution. A model for hospitalist led MDTs could be implemented at other hospitals to provide guidelines-based care of patients with tracheostomies and ideally also reduce complications and LOS.