Background: As a direct or indirect consequence of the COVID-19 crisis, staff shortages are inevitable. Hospitalists may require quarantine after significant exposure to the virus or due to illness. Census surges are anticipated as well. It is crucial to implement alternate staffing plans to prevent disruptions in patient care. Telemedicine can be leveraged as a solution to staffing shortages.
Purpose: To implement a telemedicine backup for the hospital medicine service during periods of physician staff shortages and census surges related to COVID-19.
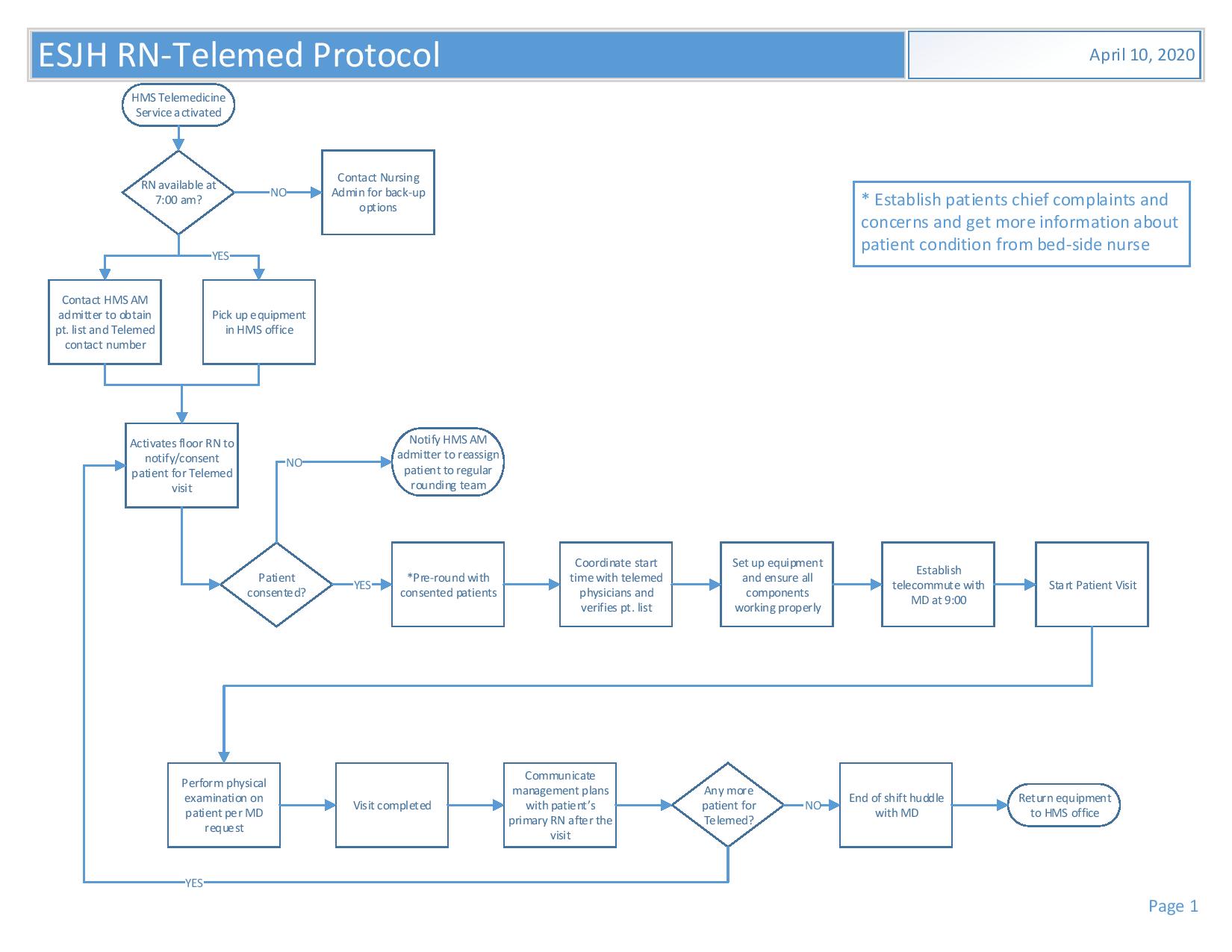
Description: Emory Saint Joseph hospital is an acute care tertiary hospital with 410 beds located in one of the largest cities in Georgia. 90% of patients admitted to the hospital are assigned to the hospital medicine service. There are 9 hospitalist teams with an average of 150 patients daily. With the COVID-19 pandemic, there is an expected increase in number of patients daily by 10-15%, as such it was imperative to develop alternate staffing plans which could be implemented rapidly, efficiently with low resource utilization. A telemedicine committee was created which included hospitalists, hospital administrators and quality officers. Weekly meetings were held to brainstorm implementation of a viable, cost-effective telemedicine service. A3 process and problem-solving approach was utilized. To mitigate potential problems with staffing, protocols and work flows were developed with guidance on when the telemedicine team would be utilized and patient selection for telemedicine. The telemedicine team would be deployed if the census average was 18 or more per team or in event of physician illness, to cover a team. Criteria for patient inclusion included established low acuity patients, medicine consults for patients with chronic stable medical conditions and stable patients awaiting placement with the goal to enable physicians onsite to be available for more complex patients.The telemedicine team included a hospitalist and a RN who served primarily as the telemedicine nurse who will be onsite and move equipment from room to room during rounds and assist the tele hospitalist with the physical exam. To conserve resources, simple equipment using a laptop, digital software using zoom and digital stethoscope was utilized. Physician and nursing training were completed. 2 successful pilots were carried out and a total of 6 patients evaluated with telemedicine. The project is currently underway and data collection ongoing.
Conclusions: An operational tele hospitalist service can be rapidly implemented during the COVID-19 pandemic using readily available equipment, as a viable solution to staffing shortages and census surges.