Background: Tracheostomies are commonly performed on critically ill patients requiring prolonged respiratory support. Managing them in intermediate care units (IMCU) presents challenges, as complications such as tube displacement, infection, and airway obstruction can pose significant risks. Structured safety protocols like checklists have been successfully used in other high-risk healthcare settings to mitigate these risks. Thomassen et al. conducted a systematic review examining the effects of safety checklists in medicine, finding improvements in morbidity, mortality, adherence to guidelines, communication, teamwork, and reduced adverse events. Similarly, Hazelton et al. introduced a safety checklist for bedside bronchoscopy-guided tracheostomies, resulting in a 580% reduction in adverse procedural events. MacKinnon et al. assessed ICU rounding checklists and found improvements in mortality, length of stay, and infection rates. These studies suggest that a standardized safety checklist for tracheostomy care in the IMCU could offer comparable benefits. Furthermore, there is limited data on variability in hospitalists’ training in and comfort with management of tracheostomy patients. A standardized checklist could help address these inconsistencies and improve care quality.
Purpose: The purpose of this initiative is to implement a tracheostomy safety checklist in an IMCU at the Johns Hopkins Hospital. The goal is to improve patient safety by increasing provider confidence in managing tracheostomy patients, improving interdisciplinary care team communication, lowering healthcare-associated infections, and improving overall length of stay.
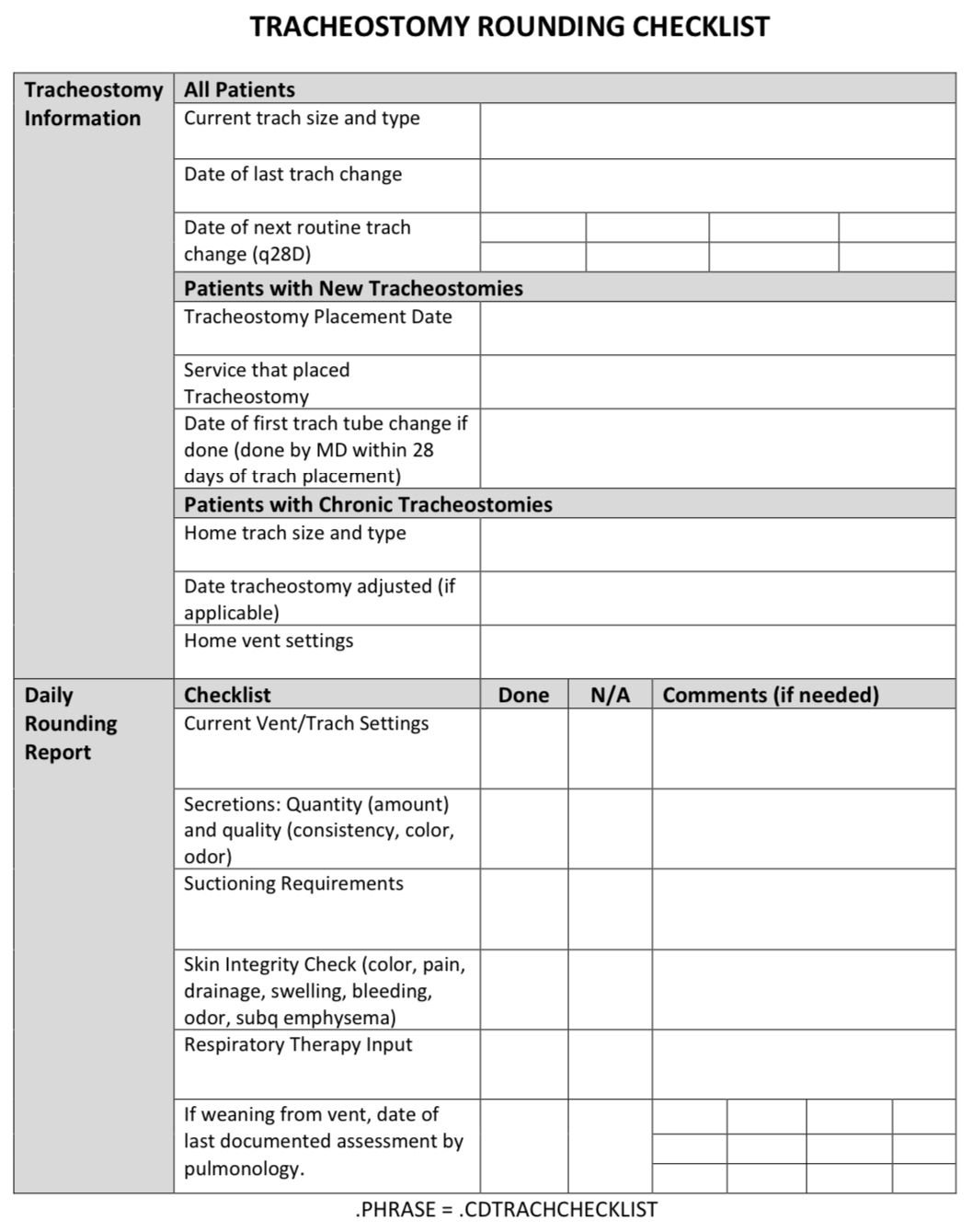
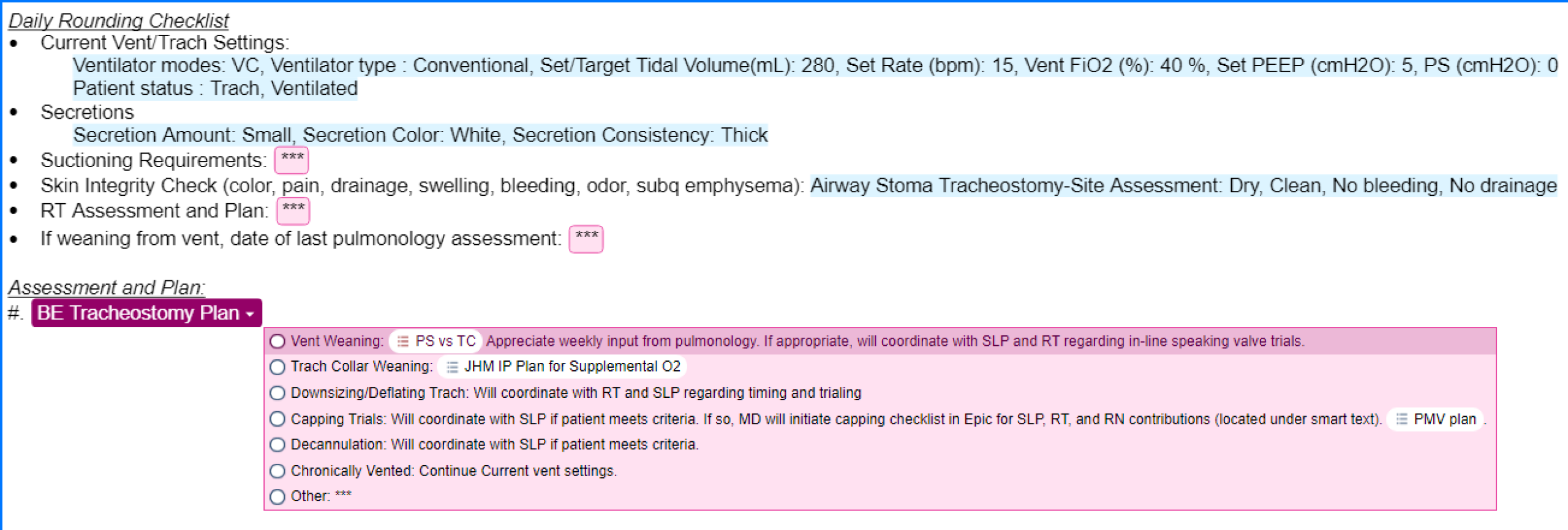
Description: A multidisciplinary team consisting of physicians, nurses, respiratory therapists (RTs), and speech-language pathologists developed a comprehensive tracheostomy safety checklist. The checklist includes key components of tracheostomy management, such as ventilator settings, tracheostomy settings, secretion quality, suction frequency, respiratory therapy assessments, and documentation of routine care (Figure 1). The checklist is designed for use during daily bedside rounds with nursing and RT to standardize evaluations and management. It was adapted into a dot phrase within the Epic system to facilitate tracking of its use and to facilitate documentation of patients’ clinical status on a daily basis. (Figure 2). Data will be collected over a six-month period to assess the impact of the checklist on adverse events, including tracheostomy tube dislodgement, upgrades to the ICU, tracheostomy-related pressure injuries, and overall length of stay. In addition, staff satisfaction with the checklist and its perceived effect on care delivery will be evaluated through surveys.
Conclusions: This initiative aims to standardize tracheostomy care, enhance provider confidence, and reduce patient safety risks in the IMCU. By collecting both objective and subjective data, we hope to evaluate the feasibility and effectiveness of a tracheostomy safety checklist in improving patient outcomes and streamlining care delivery in an IMC environment.