Background: Hospital medicine groups endeavor to avoid excessive workloads which can contribute to burnout. 1,2,3,4Groups vary in how new patients are distributed, but larger groups often assign a single hospitalist to carry an admitting pager and distribute new patients among several colleagues. This “admitting pager” role combines high volume with frequent interruptions and multitasking as the hospitalist struggles to admit new patients while also distributing admissions and coordinating reports. Internal data from our group showed the swing admitting shift was the busiest shift due to the number of admissions coming in and numerous pages regarding admissions, transfers and other questions. Carrying the admitting pager was also identified as a large stressor on our annual division survey. We sought to determine the effect of a Triage Nurse on hospitalists’ perceived workload and frequency of paging interruptions.
Methods: We partnered with our patient throughput department to implement the Triage Nurse role in May 2017 with a goal of relieving some activities of swing admitting hospitalists and reducing the number of pages received. The Triage Nurse took responsibility of tracking and distributing admissions amongst three admitting physicians along with coordinating report. We also created an algorithm to guide the Triage Nurse to handle extraneous pages and questions received to pass the necessary information to parties responsible.We used the National Aeronautics and Space Administration-Task Load Index (NASA-TLX) to measure perceived workload. The NASA-TLX is a six-item questionnaire, has been validated for use in the healthcare setting, and is used to quantify stress from physical, mental, performance and time constraints on the work of healthcare workers. We measured NASA-TLX scores of physicians on the swing admitting shift before and after implementation of an Triage Nurse. We also measured the number pages received by the swing admitters in a sample of days from the pre-intervention to post-intervention period using electronic pager logs. We compared median NASA-TLX scores using the Wilcoxon rank sum test and the mean number of pages using a t-test.
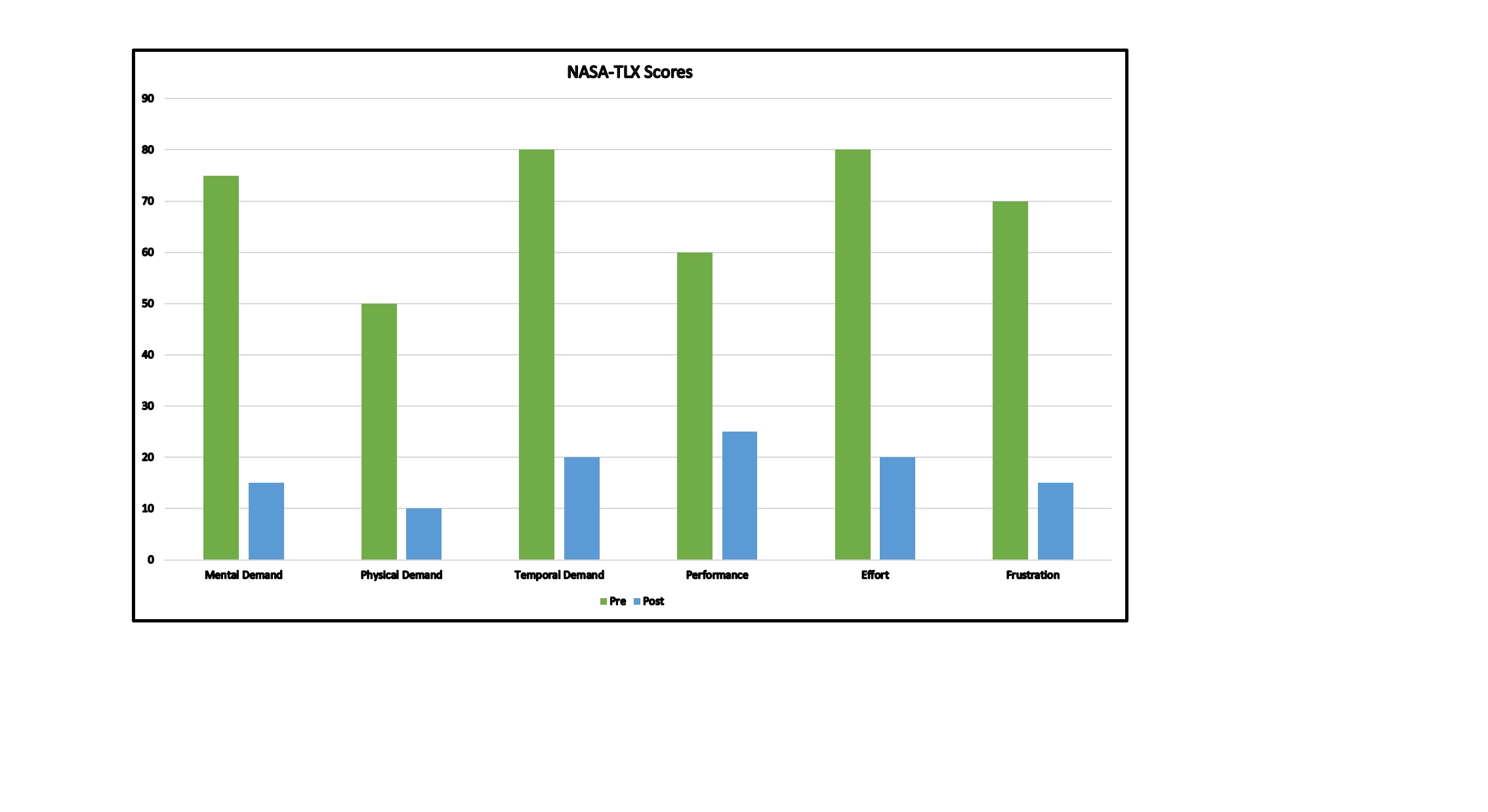
Results: We had 49 of 66 expected surveys (74%) returned in the pre-intervention period and 65 of 92 expected surveys (71%) returned in the post-intervention period. On review of NASA-TLX scores before and after implementation of the Triage RN, we found a statistically significant decrease in mental demand, physical demand, temporal demand, effort and frustration (p < 0.01) along with performance (p= 0.01) with a lower number indicative of lower workload. The number of pages decreased from a mean of 81 ± 16.6 pages in the pre-intervention pages to 52 ± 7.4 in the post-intervention period.
Conclusions: With implementation of the Triage Nurse role, the perceived workload by the swing admitting hospitalists decreased in all domains. Additionally, the number of pages received by this hospitalist also decreased. This role was identified as a positive change on our annual group survey, supporting a positive effect on wellness. While more research is needed to clarify the association between workload and burnout, the current work highlights the need for modifications in response to stressors identified by clinicians to positively impact the work of hospitalists.