Background: Total joint arthroplasties (TJA) are the most frequently performed orthopedic surgeries in the USA. Given the aging US population, the number of TJA surgeries is expected to grow by 559% by 2060. Additionally, the average medical comorbidity for patients undergoing TJA surgery is increasing, a trend that is expected to continue. Given both the rising volumes and medical complexity of patients, there is concern for patient safety and quality outcomes. Since the launch of the Comprehensive Care for Joint Replacement Model in 2016, Medicare is progressively reimbursing TJA surgeries via bundled payments that prioritize quality metrics such as length of stay, over fee-for-service models. For these reasons, there is growing interest in expanding the role of hospitalist providers in co-management of TJA patients to improve outcomes.
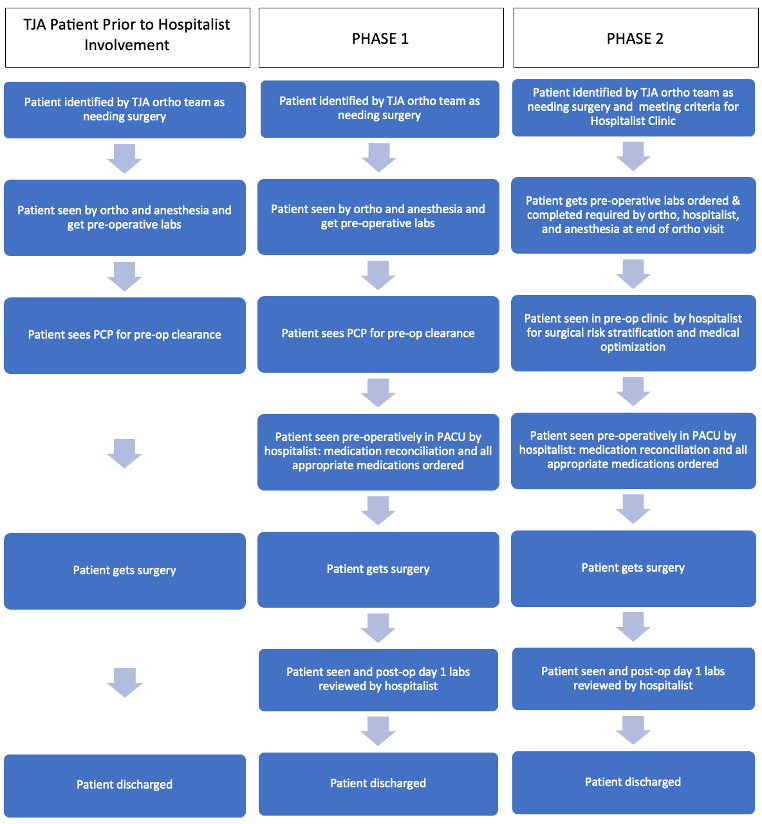
Purpose: The purpose of this clinical innovation was to create a hospitalist-led, comprehensive co-management model for the care of TJA patients at an academic medical center. This years-long effort had graduated goals: to provide full inpatient co-management services to all TJA patients admitted to the hospital after surgery and eventually to launch a hospitalist-run preoperative clinic for medically complex patients preparing for TJA. The purpose of this ambulatory clinic was to provide surgical risk assessments, perioperative medical optimization, and highlight opportunities for improved inpatient care, creating seamless co-management for medically complex TJA patients.
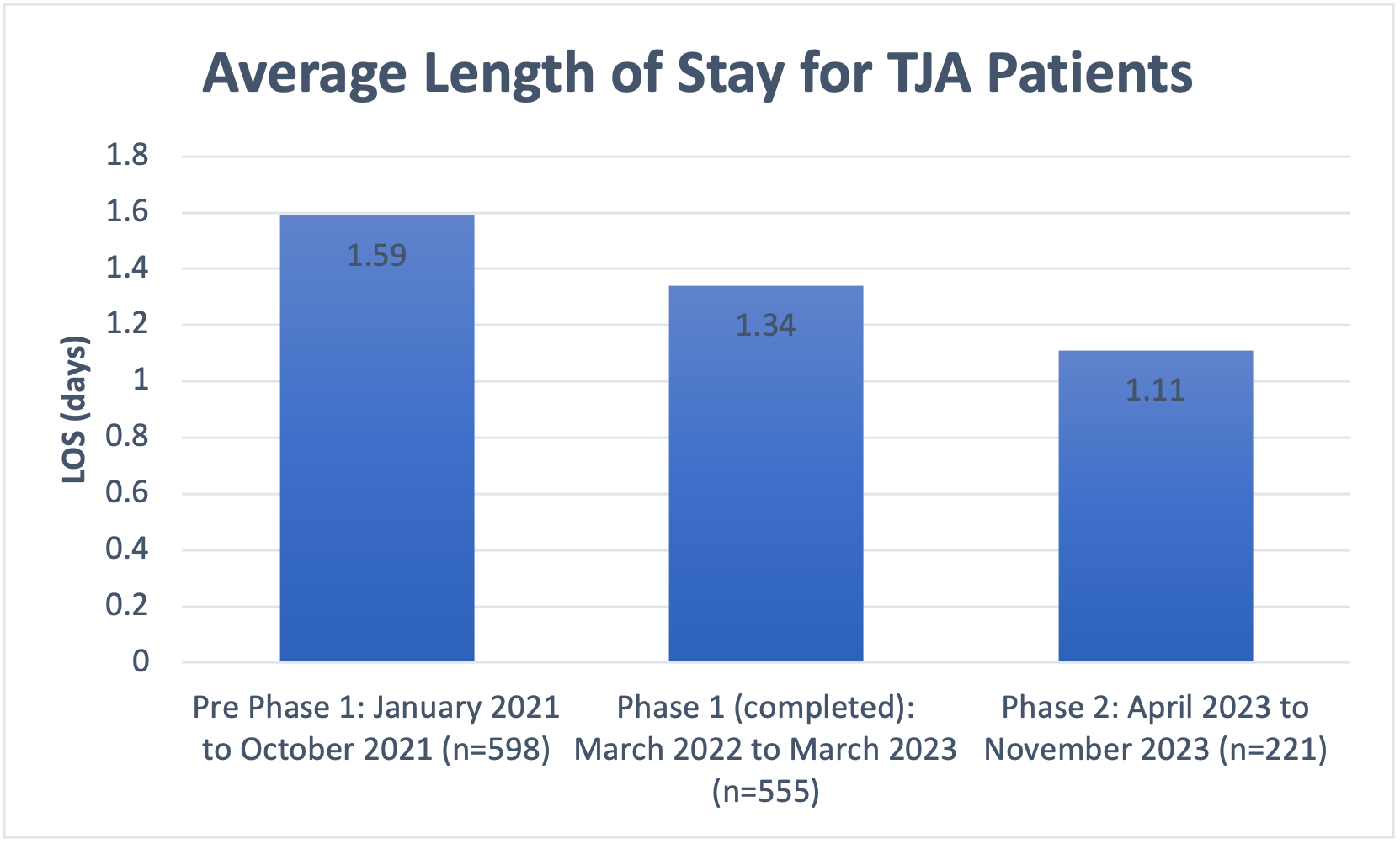
Description: In 2021 the University of Chicago created a workgroup led by the Director of the Hospital Medicine Consult Service (HMCS) and QI Director of the Department of Orthopedic Surgery focused on expanding the role of the HMCS to provide co-management services for all TJA patients admitted postoperatively. This working group began as a monthly meeting in February, later increasing its cadence to every other week. It involved project managers, QI staff, and physician and APP providers from the Department of Orthopedic Surgery as well as hospitalist champions from the Section of Hospital Medicine. A co-management contract was codified, stating that hospitalists would see all TJA patients in the PACU, complete the medication reconciliation, and order all additional medications not related to pain control or anticoagulation. Phase I began November 2021 with the co-management of two of the four TJA surgeons. The other two surgeons’ patients were incorporated in March 2022, completing Phase I. Since the start of Phase I, 555 patients received enhanced inpatient co-management care. Phase II was launched in April 2023 which saw the start of a half-day outpatient clinic staffed by the same cohort of hospitalist providers. This expanded to a full day clinic in October 2023 (Figure 1). Since the creation of the ambulatory clinic during Phase II, there has been a total of 221 patients seen in clinic. During the 10 months prior to the launch of Phase I, the average LOS for a TJA patient was 1.59 days. During the completed Phase I, the average LOS decreased to 1.34 days, and during Phase II has further decreased to 1.11 days, a 30.2% decrease since the start of co-management (Figure 2). Additionally, same day discharges improved from 29% to 34.2% during Phase II.
Conclusions: The creation of a hospitalist-led comprehensive co-management model for TJA patients involving both outpatient and inpatient perioperative care is feasible and associated with improved length of stay and increased same day discharges.