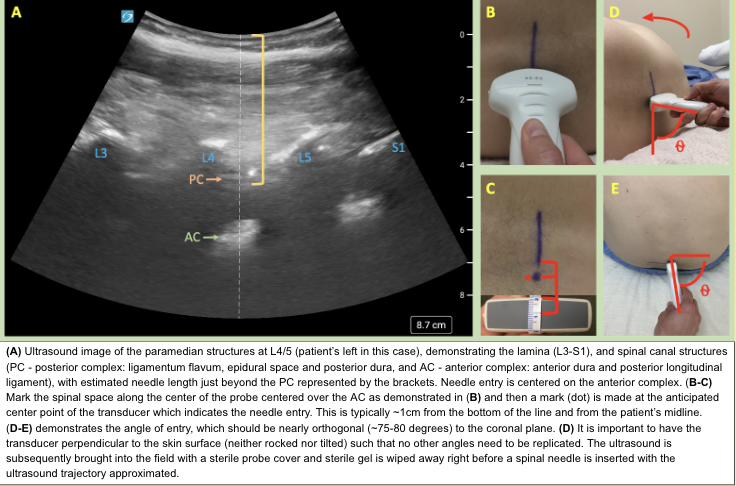
Background: Lumbar punctures (LPs) are common among hospitalized patients and many institutions have implemented a hospital medicine procedure services (HMPS) to perform these routine bedside procedures. Most clinicians learn to perform this procedure using the midline (ML), landmark-guided approach which involves palpation of the lumbar spine but this technique is associated with failure rates as high as 20-30% (1). Off-midline or paramedian (PM) approaches to LPs have been used before the incorporation of ultrasound (US). (2) An advantage of a PM approach is that the needle accesses the spinal canal via the interlaminar space which typically offers a wider aperture when compared to the interspinous space. (Fig. 1) However, the needle needs to be directed at a sagittal-oblique angle, which can be difficult to determine without the aid of US. Literature supporting a PM approach is scarce and studies often have considerable limitations with external validity. Various techniques using US assistance and real-time guidance have been shown to improve first and second pass success rates in patients needing spinal anesthesia. (3) To date there is no evidence evaluating the efficacy of an ultrasound assisted paramedian (USPM) approach to bedside LP using intra-procedural US in the acute care setting.
Methods: Design: Retrospective cohort studyTechnique Training: The USPM approach was incorporated into the HMPS practice after standardizing a self-study curriculum. Hands-on, in-service training for all proceduralists was completed with an at-the-elbow expert. Technique competency was demonstrated by 2-5 independently successful LPs. Subsequent faculty who joined the HMPS demonstrated competency prior to beginning service on the HMPS. Analysis: All LPs performed from October 2017-May 2022 were reviewed. Our primary analysis compared the probability of a successful LP after USPM technique standardization versus ML approach. We estimated the risk difference using a logistic regression model that included BMI, sex, age, and indication. We then applied this logistic regression model to compute a predicted probability of success for each of the USPM and ML approaches for every patient in our sample, plugging in patient-specific values for each characteristic in the model. We averaged these individual treatment effects across the entire sample to estimate the average treatment effect of the USPM versus ML approach. We used the “marginaleffects” package in R to implement this estimation and inference procedure
Results: The HMPS recorded 84 ML LPs over the 2 year period prior to USPM LP training and 185 USPM LPs in the period following training with success rates of 72.6 and 85.4 percent, respectively. The probability of a successful LP was 13.58% (95% CI: 2.80, 24.36 P=0.014) higher when compared to the ML approach. The odds of success for USPM vs. ML was also significantly higher (OR 2.41, 95% CI: 1.21, 4.79; P=0.012). The increased rate of success also corresponded to a decrease in use of Neuroradiology consultation (OR 0.44 95% CI: 0.22, 0.83 P=0.01). Both groups had similar periprocedural coagulation profiles, and similarly low rates of traumatic tap, post-procedural blood patch and epidural hematoma.
Conclusions: USPM LP was associated with an increased LP success rate and a reduction in neuroradiology utilization. Proceduralist groups that perform bedside LPs on hospitalized patients and who have US proficiency should consider incorporating a USPM approach to their practice.