Background:
On October 1, 2007, Medicare changed their payment structure from Diagnosis Related Group (DRG) to Medicare Severity-Diagnosis Related Group (MS-DRG) based reimbursement. This led institutions to prioritize clinical documentation improvement (CDI) programs in an attempt to align healthcare resources with patient complexity. Complete documentation has other benefits to a healthcare system as well. These include accurate reporting of risk-adjusted outcomes to quality rating organizations and accurate communication of patients’ diagnoses in the electronic health record (EHR) to improve quality of care and patient safety.
Purpose:
As a tertiary care center, our university healthcare system cares for complex patients. However, our case-mix index (CMI) and observed-to-expected (O/E) mortality rates were not in line with our peer institutions for similar patient populations. Upon further analysis, we discovered that our capture rate for many comorbid conditions was poor. Our goal was to improve provider documentation of comorbid conditions in our patients.
Description:
In February 2015, we educated providers and employed basic quality improvement techniques including standardization and error proofing. Using an EHR solution, we embedded a table of common comorbidities encountered, but often not documented on our general medicine service. Conditions included were anemia, chronic liver disease, coagulopathy, congestive heart failure, hyper- or hypokalemia, hyper- or hyponatremia, malnutrition, metastatic cancer, obesity, peripheral vascular disease, and renal disease. Providers were prompted to toggle through “Yes/No” fields for each of the above conditions with relevant laboratory and vital sign data automatically referenced where appropriate.
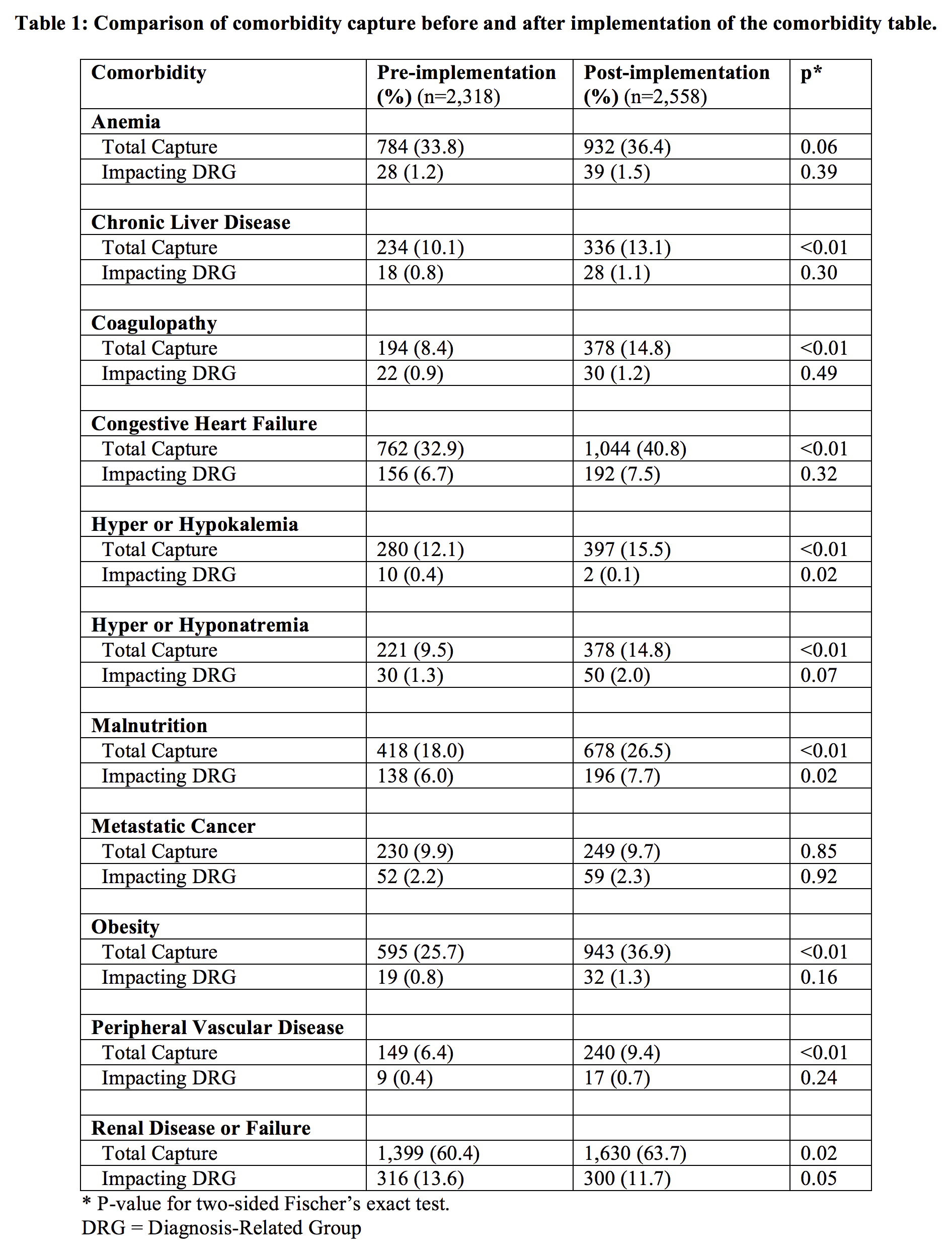
To understand the intervention’s impact, we compared coding data before and after implementation. For the 8 months post-implementation, we saw a statistically significant (p < 0.05) increase in capture rates for 9 of the 11 comorbidities (Table 1). Additionally, we found significantly increased capture of malnutrition, potassium disturbances, and renal disease in cases where DRG weighting was impacted (p-values 0.02, 0.02, and 0.05, respectively).
Conclusions:
By embedding a comorbidity table into existing note templates, we demonstrated sustained improvement in comorbidity documentation using basic quality improvement techniques. This positively impacted patient care and public reporting of patient complexity. Overall, capture improved for nearly all of the comorbidities included, with 3 conditions resulting in a significant impact to MS-DRG weighting. Further work will aim to adapt this proof-of-concept to other settings where accuracy in clinical documentation is important.