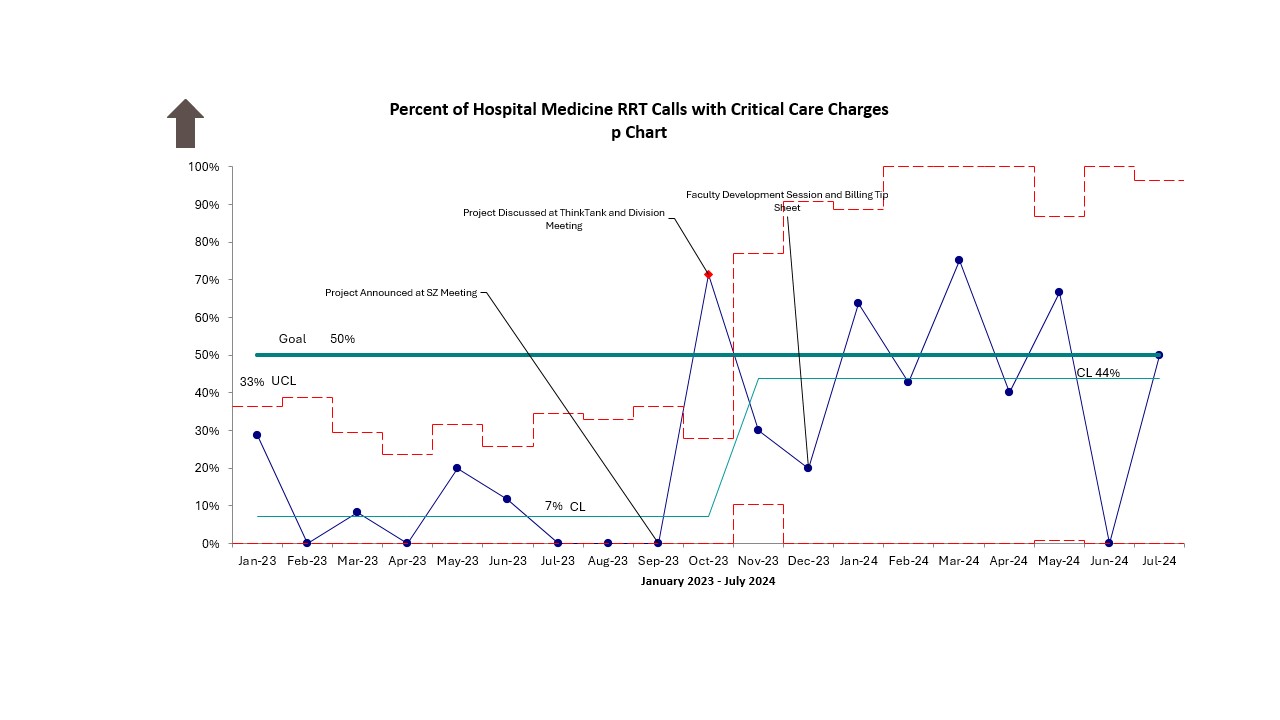
Background: Professional billing is crucial for both division revenue and sustainable healthcare. However, provider knowledge on optimal billing for varied clinical scenarios is often lacking. Critical Care Current Procedural Terminology (CPT) Evaluation and Management (E/M) codes are often appropriate for Hospital Medicine (HM) providers to use when providing critical care services to patients during a rapid response call, however baseline data showed that these codes are underutilized. Our specific aim was to increase use of Critical Care CPT E/M codes by the HM division for patients meeting critical care criteria and for whom a rapid response was called from 7% to 50% within 10 months and sustain for 6 months.
Methods: This quality improvement effort was conducted from January 2023 through July 2024 in a 320 bed, free standing, children’s hospital. The Hospital Medicine division has an average morning census of approximately 50 patients managed by residents, fellows and attendings. All daytime, weekday rapid response calls to the Hospital Medicine service were included. A chart review of those calls was conducted to verify critical care criteria was met, to identify which charges were placed and to review the documentation to ensure it met the Centers for Medicare and Medicaid (CMS) requirements. Interventions included educational sessions, a tip sheet, improved access to billing codes in the EMR, and regular data updates.
Results: Critical Care CPT E/M code usage increased from 7% to 44%. When a Critical Care CPT E/M code was used, retrospective chart review demonstrated the patient met critical care criteria 100% of the time and had appropriate documentation to support use of the code 67% of the time. During the intervention period, 73 critical care charges were placed, leading to an additional $10,590.84 cumulative charges captured.
Conclusions: Educational interventions, just-in-time resources, and regular feedback on professional billing improve appropriate critical care billing code utilization and optimize revenue to better reflect the variety and complexity of care provided. Next steps include expanding to non-daytime hours, optimizing provider documentation, and applying this work to other sites within our regional network.