Background:
Patient handoffs at physician shift changes are limited in their ability to convey the insight that the primary team has gained by longitudinal personal care of the patient. The Patient Acuity Rating (PAR) is a previously validated 7‐point Likert score quantifying physician judgment regarding how likely a patient is to suffer a cardiac arrest or require emergent transfer to the ICU in the next 24 hours (with 7 being extremely). However, its impact on cross‐covering physician assessment and management of patients is not known. We hypothesized that interns would modify their level of concern and need to go the bedside in accordance with this tool and that the utility of the PAR utility would vary with intern experience.
Methods:
Experienced (May/June) and novice (July) intern physicians were surveyed using 10 real, randomly chosen, deidentified patient sign‐outs that had previously been assigned PAR scores by their respective primary teams. They were instructed to read the sign‐out, assign a PAR score to it, and then answer several questions, using a 5‐point Likert scale regarding a hypothetical cross‐cover scenario with progressive borderline tachycardia. Questions included “How concerned are you about the stability of this patient?” and “How important is it that you go to the bedside to evaluate this patient right away?” (with 5 being extremely). The primary team PAR score was then revealed, and the subjects answered the same questions. This process was repeated for each of the 10 patients. Responses were compared using paired and unpaired 2‐sided / tests, as appropriate. Linear regression was used to quantify the impact of PAR discrepancy and adjust for intern experience.
Results:
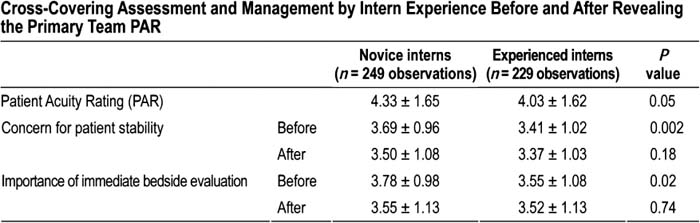
Between May and July 2008, 23 of 39 experienced interns (59%) and 25 of 42 novice interns (60%) answered questions involving 478 patient scenarios. The mean PAR score assigned by the study interns was 4.2 ± 1.6 vs. 3.8 ± 1.8 for the primary teams (P < 0.001). The mean concern for patient stability decreased from 3.6 ± 1.0 to 3.4 ± 1.0 IP = 0.006) after revealing the primary team PAR, whereas the urgency of bedside evaluation decreased from 3.7 ± 1.0 to 3.5 ± 1.1 (P = 0.003). The table shows the results broken down by experience. The regression coefficients for the changes in concern and urgency with PAR discrepancy were 0.32 (P < 0.001), without any significant differences based on experience.
Cross‐Covering Assessment and Management by Intern Experience Before and After Revealing the Primary Team PAR
Conclusions:
Experienced interns better predict the primary team's PAR. When there is a discrepancy between the primary and subject PARs, interns of all experience levels modify their level of concern and need to go to the bedside in the direction of the primary team's PAR score. Provision of the PAR score eliminated the differences in level of concern and urgency of bedside evaluation between novice and experienced interns.
Author Disclosure:
D. Edelson, Philips Healthcare, research grant, consulting, speaking honoraria; American Heart Association, research grant.