Background: Studies have demonstrated direct discharge to home with home care after hospitalization to be the optimal strategy for patients with social support. Even amongst sicker patients requiring intensive nursing and therapy services, evidence shows no difference in functional recovery when compared to those discharged to inpatient rehab. Furthermore, discharge location does not result in a difference in pain, functional outcomes, or patient satisfaction. Through early interventions to prevent functional decline, we aimed to improve our institutional rates of discharges to home rather than subacute rehab (SAR) following hospitalization on one medical unit by 10% over a 3 month period.
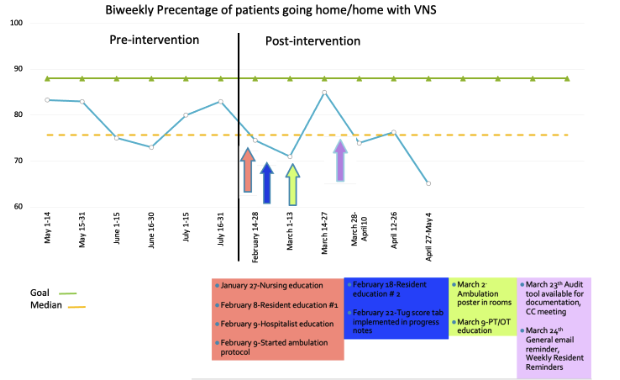
Methods: A chart review was conducted over a 3 month period to establish baseline rates of discharges to home and SAR, and to identify contributing factors for each discharge location. We piloted our project on one medical unit. An ambulation policy was created, which indicated patients meeting criteria should ambulate at least twice per day and eat out of bed at meal times. Patients were screened with the timed up and go (TUG) score and if scored below 14, were included in the program. Nurses and doctors reminded patients daily to meet ambulation goals and documented counseling via an audit tool/mobility chart. Mobility posters were placed in each patient room (in English, Spanish and Korean) as visual reminders. TUG score and nursing mobility chart documentation rate was calculated to evaluate compliance with ambulation policy. The balancing measures studied pre and post intervention included number of falls, 30 day readmission rates, average length of stay (LOS) and employee satisfaction. Several educational sessions were held with residents, nurses, physiotherapists, and hospitalists.
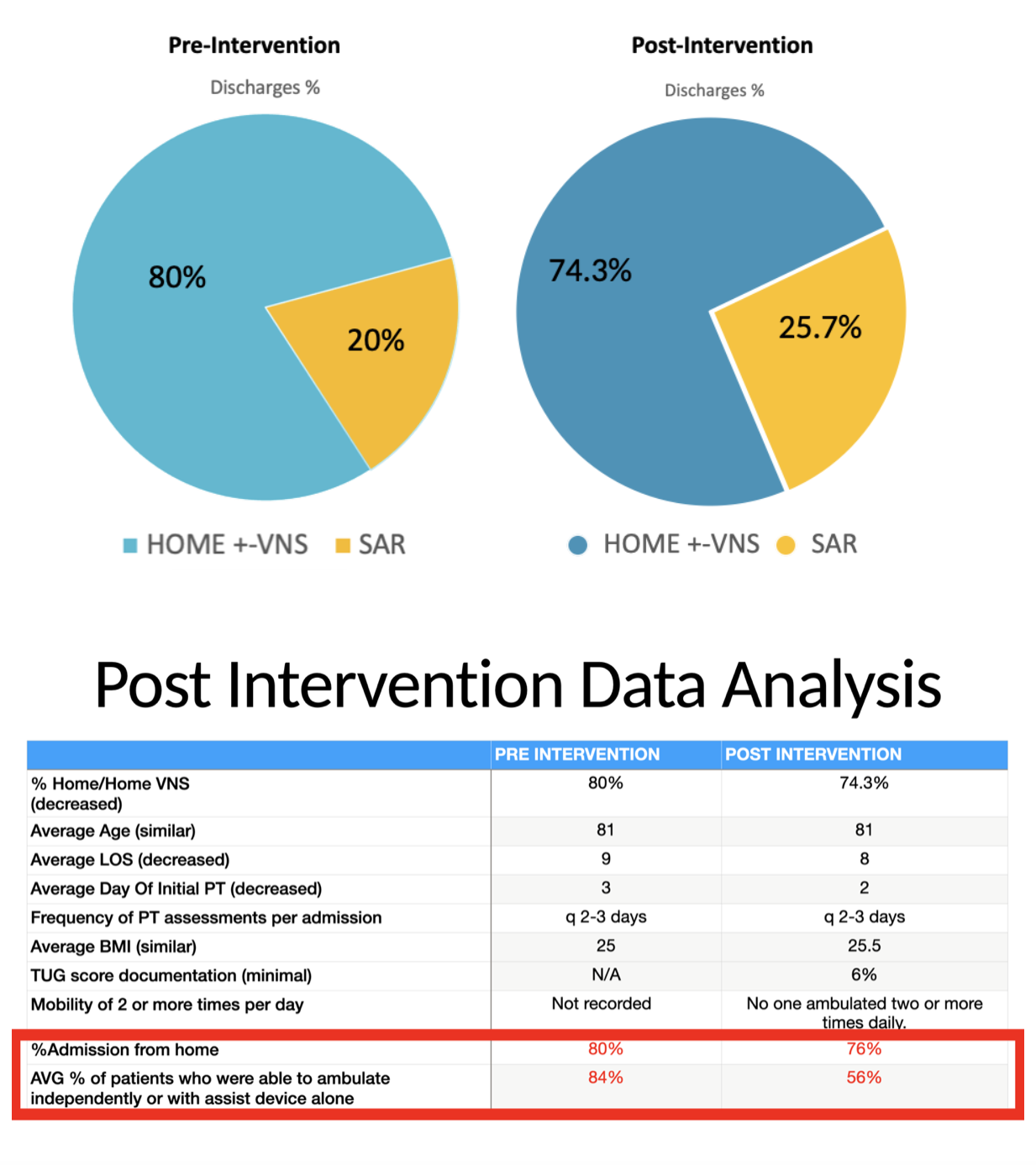
Results: Pre and post intervention data are as seen in Figure 1. From pre-intervention data, we recognized that of the patients discharged to SAR, the majority were elderly and at risk for rapid deconditioning. These patients had a long LOS and most were independent or using an assist device at admission. Post-intervention, balancing measures showed 6 falls, 16% 30- day readmission rate from home, 8 days average LOS and 80% employee satisfaction rate, with hospitalists and residents surveyed. Our post-intervention survey (n=25) assessed perceived difficulty of work flow changes for which the majority found it neither easy nor difficult (42.3%), followed by difficult (30.8%). We also assessed awareness of our project (96.2%). Major limitations included significant workflow changes, poor compliance with changes and documentation, fear of in-hospital falls with independent ambulation, multiple recommendations by physical therapy (PT) for discharge destination and limitations in staffing. Post-intervention, less patients came from home (4% difference) and less patients were able to ambulate independently or with assist devices (28% difference). At baseline, this patient population was less mobile and independent which may have impacted our outcome.
Conclusions: Disposition to home rather than SAR requires teamwork and a cohesive approach by all healthcare providers. Adoption of an ambulation policy may assist with early mobilization of patients, however compliance is crucial. Looking ahead, as our hospital plans to implement interdisciplinary discharge planning rounds, we anticipate more ease with reaching our aim. Finally, we suggest implementation of the ambulation policy via initial PT assessment.