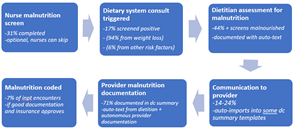
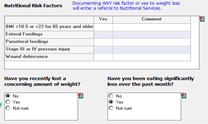
Background: Malnutrition is a significant indicator for illness severity and expected mortality. Prior to any process improvement interventions in 2014, only 4.7% of UNMH inpatients were diagnosed with malnutrition at discharge, much lower than the published national inpatient prevalence of 20-50%. Given the relatively high level of poverty in NM, we believe these lower rates reflect under-diagnosis. To improve the capture of malnutrition, an interdisciplinary process improvement team and performed the following interventions:-11/2014: created a consensus guideline to align coders and documentation practices-1/2016 : created a dietitian guideline for malnutrition screening and documentation-1/2017: revised nurse nutrition screening to include dietary consult triggers for malnutrition risk factors -9/2017: trained dietitians and providers to improve malnutrition communication and documentation -3/2022: trained dietitians to enter malnutrition diagnoses and supporting language into Powerchart and auto-importing this text into provider discharge summaries.
Purpose: To measure the impact of changes in consultation and documentation practice on coding of malnutrition.
Description: Provider Malnutrition Documentation increased as the process improvements were implemented: 8/2019-11/2019 , N=237 malnourished – 60% documented in discharge summary 10/2021-12/2021, N=216 malnourished – 64% documented in discharge summary 3/2022-5/2022, N=224 (after new dot-phase process began) – 71% documented in discharge summaryAuto importing tools also increased the percentage of documentation in the discharge summaries: 3/22: 17% 4/22: 24% 5/22: 14%Percent of encounters w/ malnutrition codes -2014: 4.7% any dx, 1% severe -2022: 7% any dx, 4.5% severe
Conclusions: Our process improvement interventions improved coding for malnutrition. However, our rates remain lower than the national average, which indicates that we are continuing to underdiagnose this important condition. Failures of malnutrition screening and diagnosis are likely causing an underestimation of mortality rates at UNMH, inflation of the mortality index at UNMH, and loss of revenue for the hospital. Lack of dietitians limits this project, as improved screening could overwhelm staffing. Next Steps: -Recruit more dietitians-Make nurse malnutrition screen a mandatory form-Alter screen so “eating less then usual” triggers system consult-Standardize discharge templates