Background: Accurate and reliable medication reconciliation (MedRec) is an indispensable step ensuring patient safety and minimizing medical errors during transitions of care. Yet, it is one of the most challenging aspects in healthcare quality and safety. In fact, inaccurate MedRec accounts for 40 % of medication errors, up to 20% of which result in harm
Purpose: To increase and maintain rate of accurate MedRec completion at MD Anderson Cancer Center (MDACC), within 24 hours of admission, to >95% utilizing performance improvement methodology.
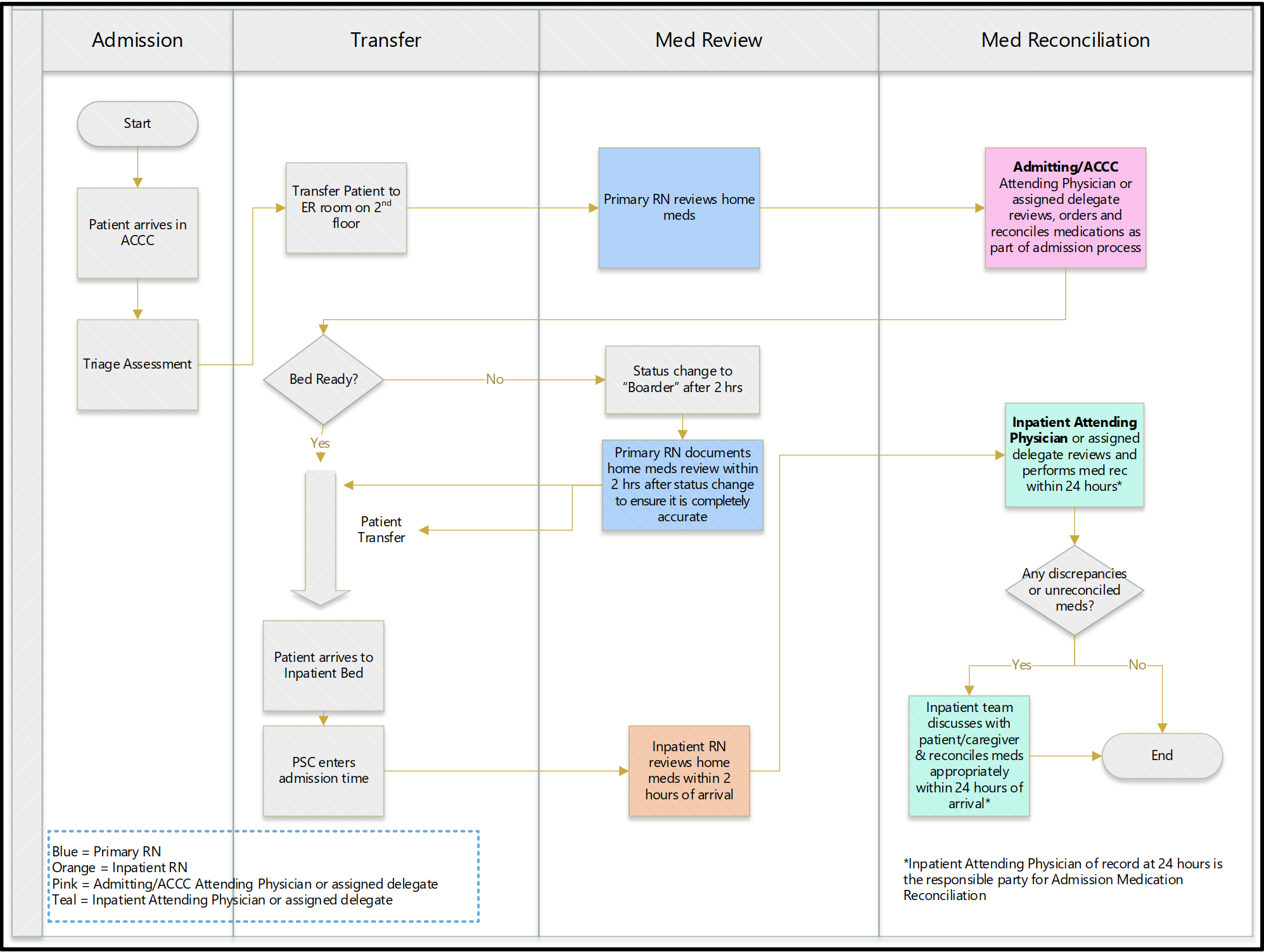
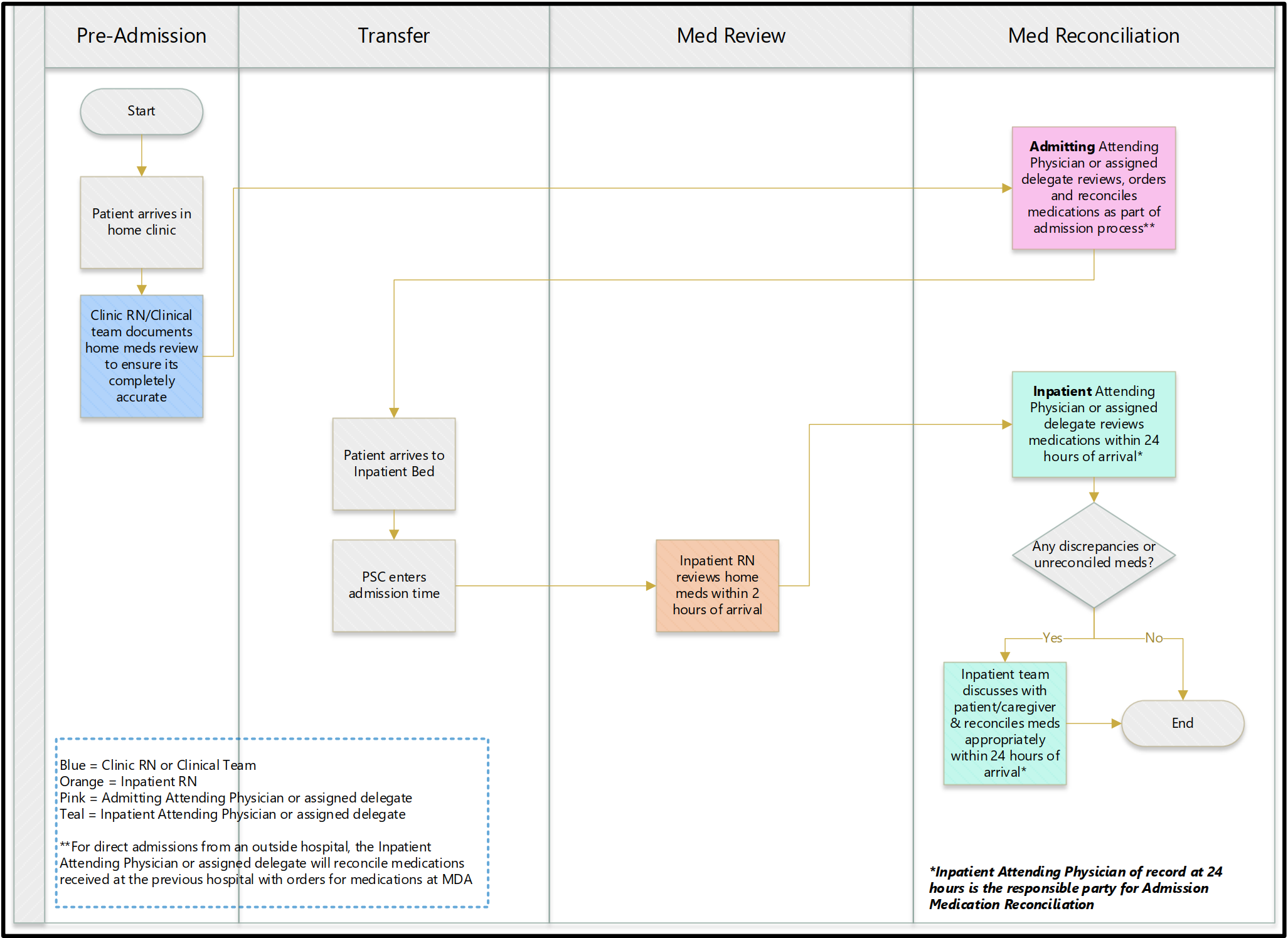
Description: Our project team included members from MDACC leadership, pharmacy, nursing leadership, IT, hospital medicine, nephrology, division of surgery and pediatrics. Our strategy consisted of 3 phases, with the first phase including 4 steps: to outline current process, to recognize challenges, to create a new process, and finally to develop a training plan. We understood that our project involved various and heterogenous medical services and departments which applied and followed varying steps in completing accurate MedRec. Therefore, to incorporate all services and departments at MDACC, we divided our project team members into medical subspecialty-based subgroups. We conducted several meetings with inpatient medical directors (IMDs) and representatives from pharmacy and IT. IMDs and department representatives provided a workflow process map of their current MedRec process.Results: Twenty percent of the records did not meet 24-hour compliance. Undefined accountability and absence of standardized accurate MedRec completion strategy were among the main reasons behind low accurate MedRec rate. Action plan: In addition to revising our institutional policy, our team developed two process maps, representing high-level workflows. We allowed an assigned delegate (Pharm D or APP) the privilege to complete MedRec, but emphasized that the inpatient attending is solely accountable for MedRec completion. IMDs have created departmental teams and customized workflows. Their essential mission is to monitor their department MedRec progress. Our IT (EPIC) team members implemented system enhancements to more easily identify MedRec status and identify compliance gaps on a service and provider level to facilitate accountability. Furthermore, a new training program was distributed to IMDs and services champions to share with their services teams. Subsequent phases of the project will continue to identify barriers, focus on transfer and discharge MedRec processes (phase 2) and ultimately focus on the accuracy of the medication list, incorporating patients and ambulatory practitioners (phase 3).
Conclusions: Accurate MedRec is a multi-phased process that requires a high level of accountability and acknowledgment of responsibility. A definite policy and proper training can reduce the likelihood of medication errors that arise during patients’ admissions or transfers of care.