Background: Self-directed discharges, also referred to as discharge “against medical advice” (AMA), refer to when patients leave the hospital prior to medical readiness. These discharges lead to worse health outcomes for patients, ethical dilemmas for clinicians, and increased readmission rates affecting healthcare systems. Research on self-directed discharges has emphasized patient characteristics affecting discharge, with less focus on nurse and physician perspectives. Studies that do explore clinicians’ roles in self-directed discharges largely draw from patient charts rather than direct interviews and focus mainly on physicians or advanced practice providers. Our study used interviews to better understand hospitalists’ and nurses’ perspectives on self-directed discharges.
Methods: We recruited hospitalists and nurses who were on a shift at our academic hospital to participate in 15-minute interviews on self-directed discharges. We conducted ten semi-structured interviews and one focus group between August and November of 2024. A total of 6 hospitalists and 11 nurses participated in our study. We used rapid qualitative methods to analyze responses and summarize key takeaways.
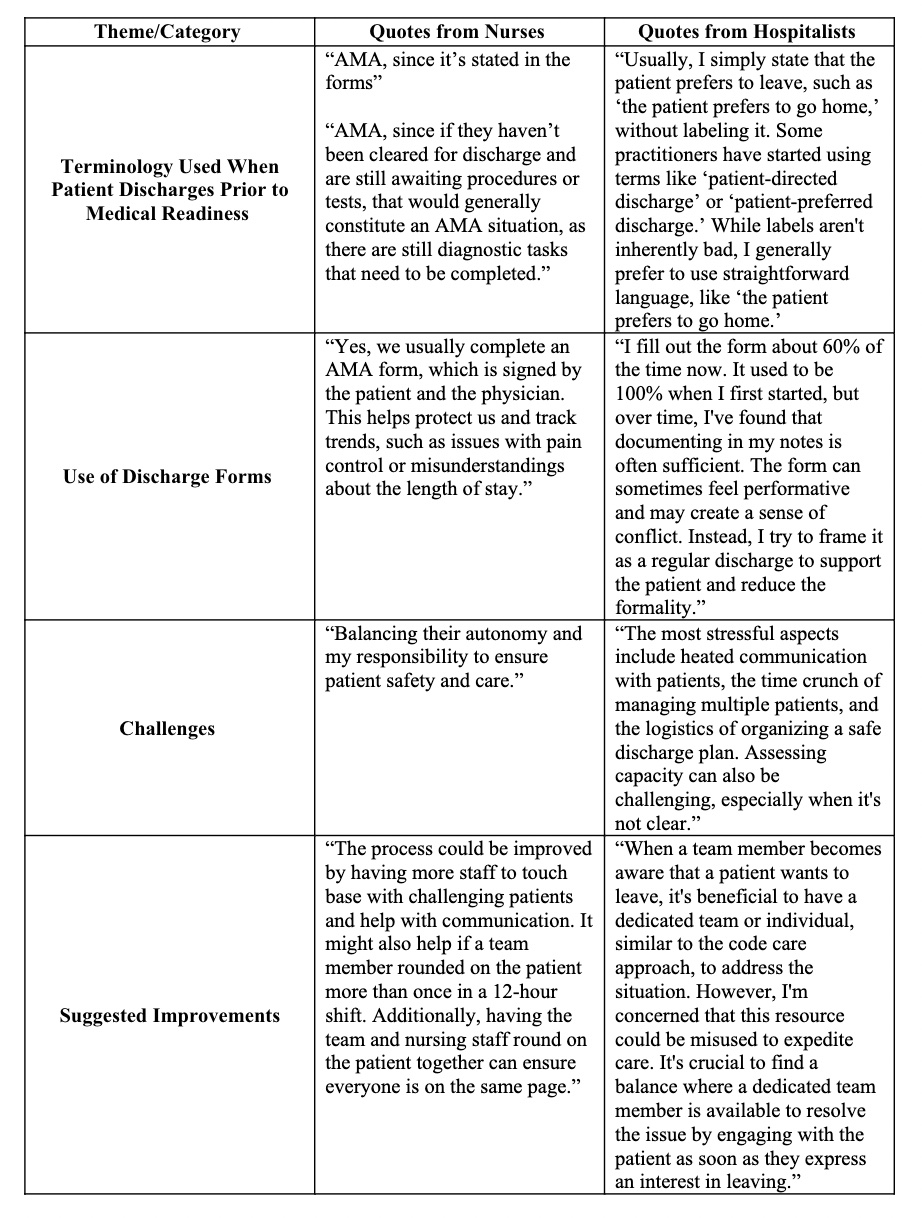
Results: Representative quotes are included in Table 1 below. Nurses were more likely to describe circumstances in which patients chose to leave the hospital prior to medical readiness as “AMA” and were more likely to emphasize the importance of completing an “AMA” form. Hospitalists preferred terms such as “self-directed discharge”. Moreover, hospitalists were less likely to formally sign any written documentation, citing concerns that this aggravates the situation. Hospitalists had variable uncertainty regarding whether signing a form was required by hospital policy. There was unanimous agreement that these discharges are often emotionally charged. Participants cited ideas to improve the self-directed discharge process such as education around self-directed discharges (e.g., legal and ethical consequences, awareness of signs indicating that patients want to leave). They also suggested a dedicated team to work with patients who express interest in leaving but noted that this measure could have the potential to perpetuate paternalism and discrimination. Nurses requested more prompt communication from hospitalists when a patient expressed interest in self-directing their discharge.
Conclusions: Hospitalists and nurses uniformly agreed that self-directed discharges create challenges and stress. There was practice variability and uncertainty around policies regarding self-directed discharges. Our findings point to the need for more education around and standardization of self-directed discharge documentation. Further understanding of patients’, nurses’, and physicians’ perspectives is crucial to improving the process of self-directed discharges in a manner that optimizes safety, collaboration, and mutual understanding and respect between all stakeholders.