Background: Physical (PT) and Occupational therapy (OT) are valuable entities, but are overused in hospitals. There is limited published literature on the appropriate utilization of PT and OT evaluations in hospitals. Analysis of all PT/OT referrals for 2018 at NewYork Presbyterian Weill Cornell showed that PT/OT orders were part of the admit order set. These orders are placed without a full understanding of their necessity. The majority of these orders are placed by night admitting teams causing unnecessary consults delays for patients with true need for PT/OT assessments. Communication was an additional barrier between the medical and PT/OT teams as PT/OT often recommended sub-acute rehabilitation and skilled nursing facility placements without a full understanding of family dynamics, patient’s insurance, financial status, and patient/family wishes. Our goal was to decrease the overall number of PT/OT consults by 10% and improve communication amongst interdisciplinary teams.
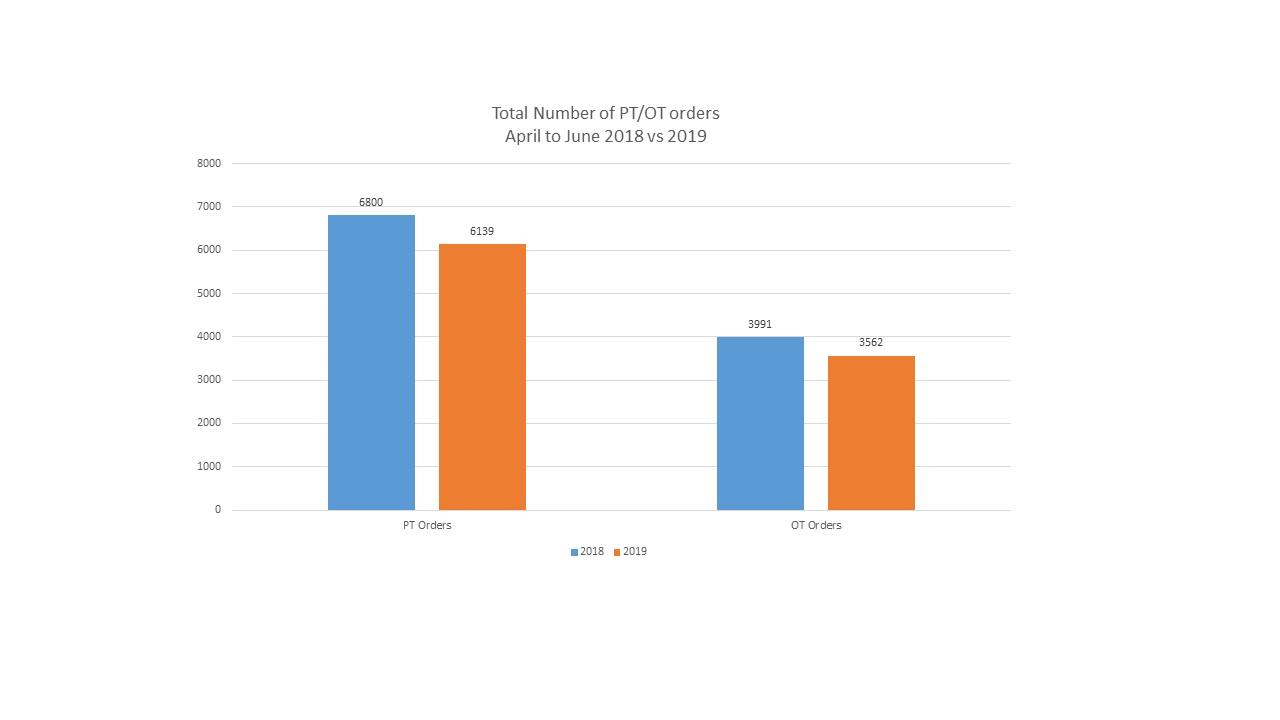
Purpose: In 2018 at NYP Weill Cornell, there were a total of 17,047 admissions to the medicine service with 6,800 (39.9%) physical therapy and 3,991 (23.4%) occupational therapy orders placed. Our goal was to decrease the overall number of PT/OT consults by 10% as well as improve communication amongst the interdisciplinary teams (ex. PT/OT, medical teams, and social work/care coordination).
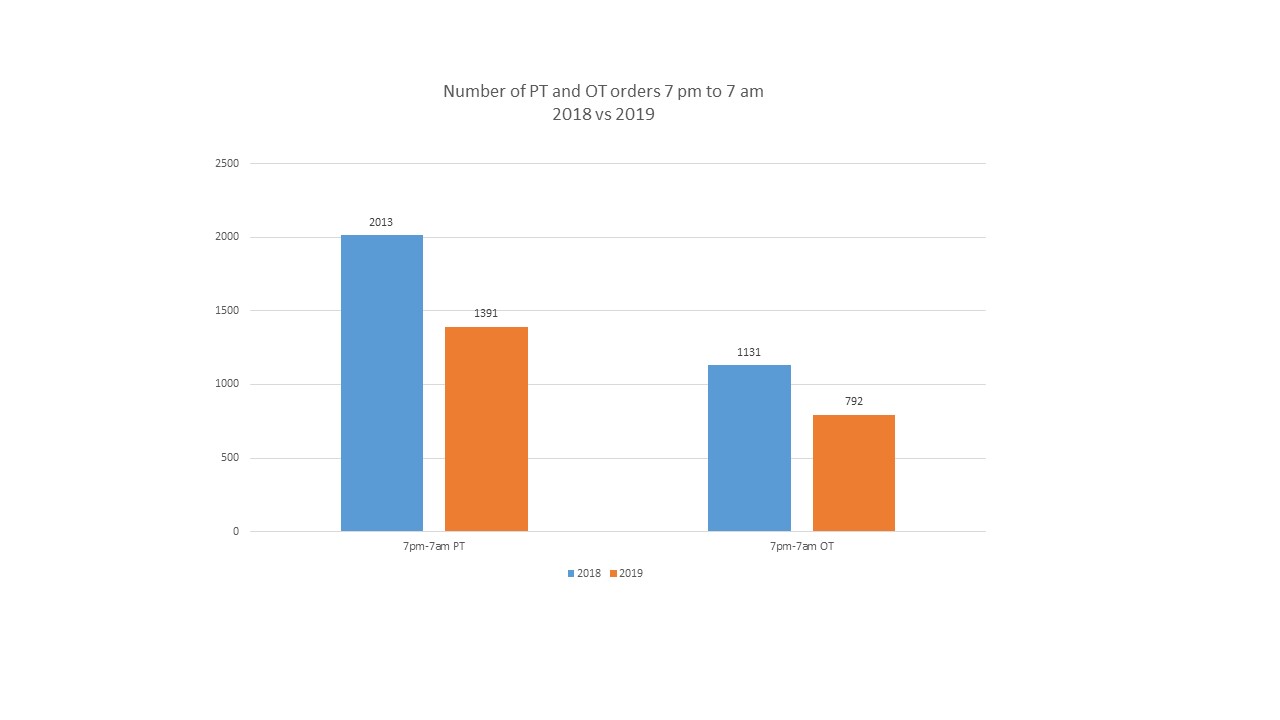
Description: In April 2019, we conducted a 3 month pilot on medicine patients to decrease the total number of PT/OT orders by 10%. We worked with IT to remove the PT/OT orders from the admission order set to ensure that consults were appropriately placed. We provided formal education for night admitting teams regarding appropriateness of placing PT/OT consults. Furthermore, on hospital day 1, patients were reviewed during interdisciplinary rounds to discuss the appropriateness of PT/OT consults. Lastly, to optimize communication, PT/OT discussed influencing factors with the interdisciplinary team prior to making final recommendations. We compared the number of consults placed pre-intervention to post intervention from April to June 2018 versus 2019. The total admissions to medicine in 2018 was 17,047 compared to 17,184 in 2019, with 39.9% of patients receiving PT consults and 23.4% with OT consults. The number of PT and OT orders decreased from 6800 to 6139 and 3991 to 3562, respectively. We further divided consults from 7 am to 7 pm and 7 pm to 7 am, as this reflects the change in shift and teams. As expected, the number of PT and OT orders from 7 am to 7 pm did not show a significant difference. However, the number of PT orders from 7 pm to 7 am decreased from 2013 to 1391 with a statistically significant difference (p value <0.0002), and the number of OT orders from 7 pm to 7 am decreased from 1131 to 792 (p value <0.03).
Conclusions: Physical and occupational therapy are critical for optimizing patient flow and throughout. Improving this process decreases delays in patient disposition to home and SNF/SAR. Although this pilot was implemented over a three month period, it has already shown a significant and lasting impact. Futures goal for our study includes analyzing the effect on length of stay and expanding this initiative to other NYP hospitals.